Ebstein anomaly
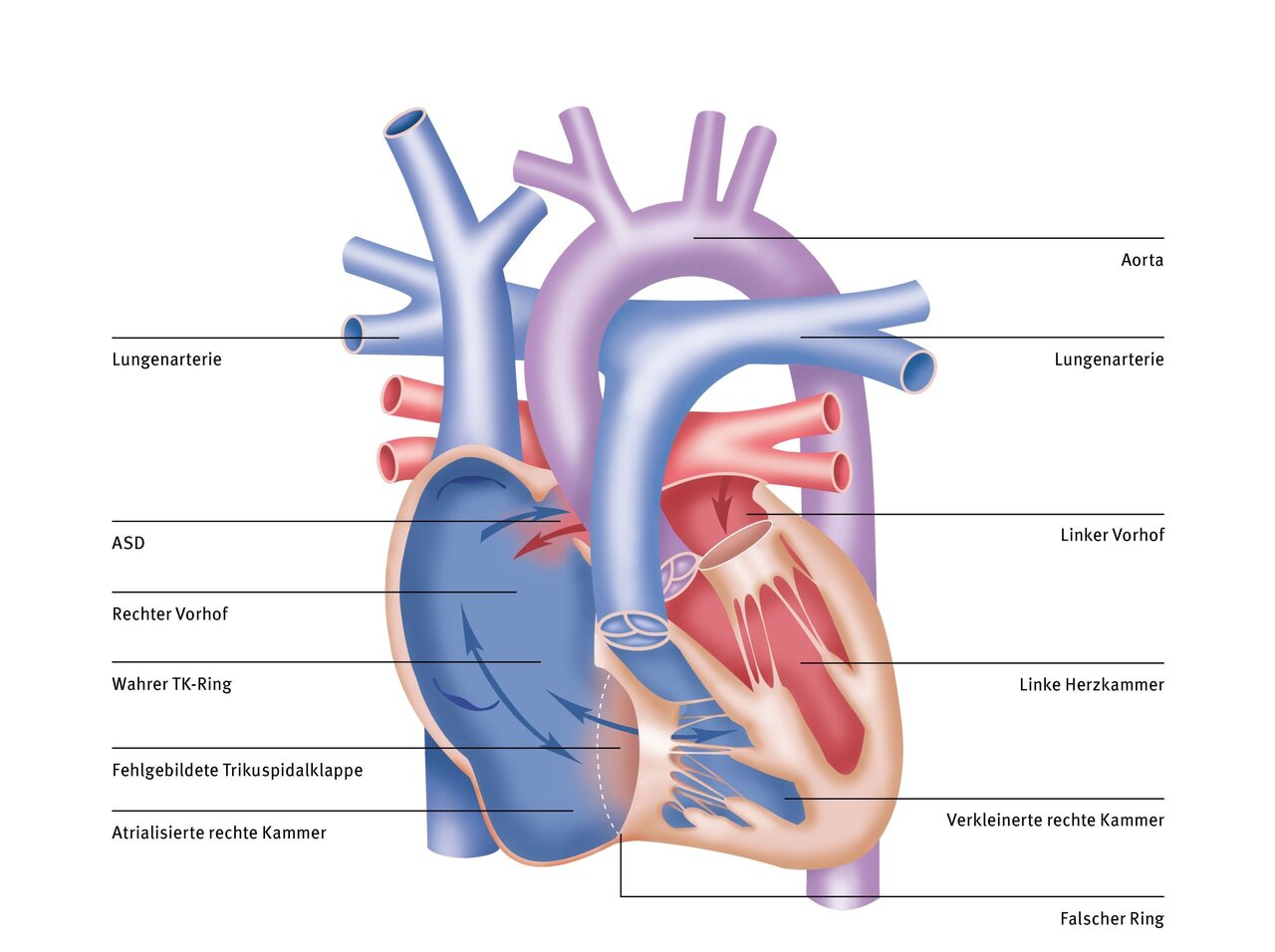
Ebstein's anomaly is a very rare congenital heart defect that is associated with a malformed tricuspid valve and an often very thin-walled right ventricle. The tricuspid valve is the ‘valve’ between the right atrium (RA) and the right ventricle (RV), which prevents the backflow of blood. The pumping capacity of the thin-walled ventricle is often restricted by the malpositioned tricuspid valve. The leaky tricuspid valve causes a back and forth flow between the right atrium and the right ventricle.
Symptoms
If the disease is mild, those affected usually do not notice it. If Ebstein's anomaly is severe, they may suffer from the following symptoms:
- Irregular and unusually strong heartbeats
- shortness of breath
- Difficulty drinking
- oedema
- Swelling of the liver
- Accumulation of fluid in the abdominal cavity
- Bluish discolouration of the skin
- Cardiac arrhythmia
Risks
As long as your child has few or no symptoms, surgery is not necessary at first. Under close pediatric cardiological supervision, it is possible to wait until adolescence or even adulthood. However, if the Ebstein anomaly is more severe, the greatest risk is right ventricular failure and the development of cardiac arrhythmias. Finally, there is a risk of stroke due to an often accompanying atrial septal defect (ASD). If thrombosis (i.e., a blood clot) occurs, for example in the leg, it can be carried in the bloodstream to the heart and, in rare cases, enter the left ventricles through the ASD. From there, in the worst case, it can be carried by the bloodstream into the cerebral vessels and block a cerebral vessel. The resulting reduced blood flow to part of the brain is called a stroke.
Echocardiography (heart ultrasound) shows the malformed tricuspid valve and the displacement of the valve into the right ventricle. This examination can be used to assess how leaky the valve is and how well the heart can pump.

Diagnosis
For diagnostics, our doctors first use echocardiography and an electrocardiogram (ECG) to determine the right heart strain. They also often carry out an additional cardiac catheterisation.
Therapy
The need for surgery will depend on the severity of the leak in the tricuspid valve and the restriction of the pumping function of the right ventricle. If an atrial septal defect (ASD) is often also present, cyanosis and cardiac arrhythmia or cardiac insufficiency and embolisms may make surgery necessary. Surgical treatment may therefore be necessary in the neonatal period or only in adulthood.
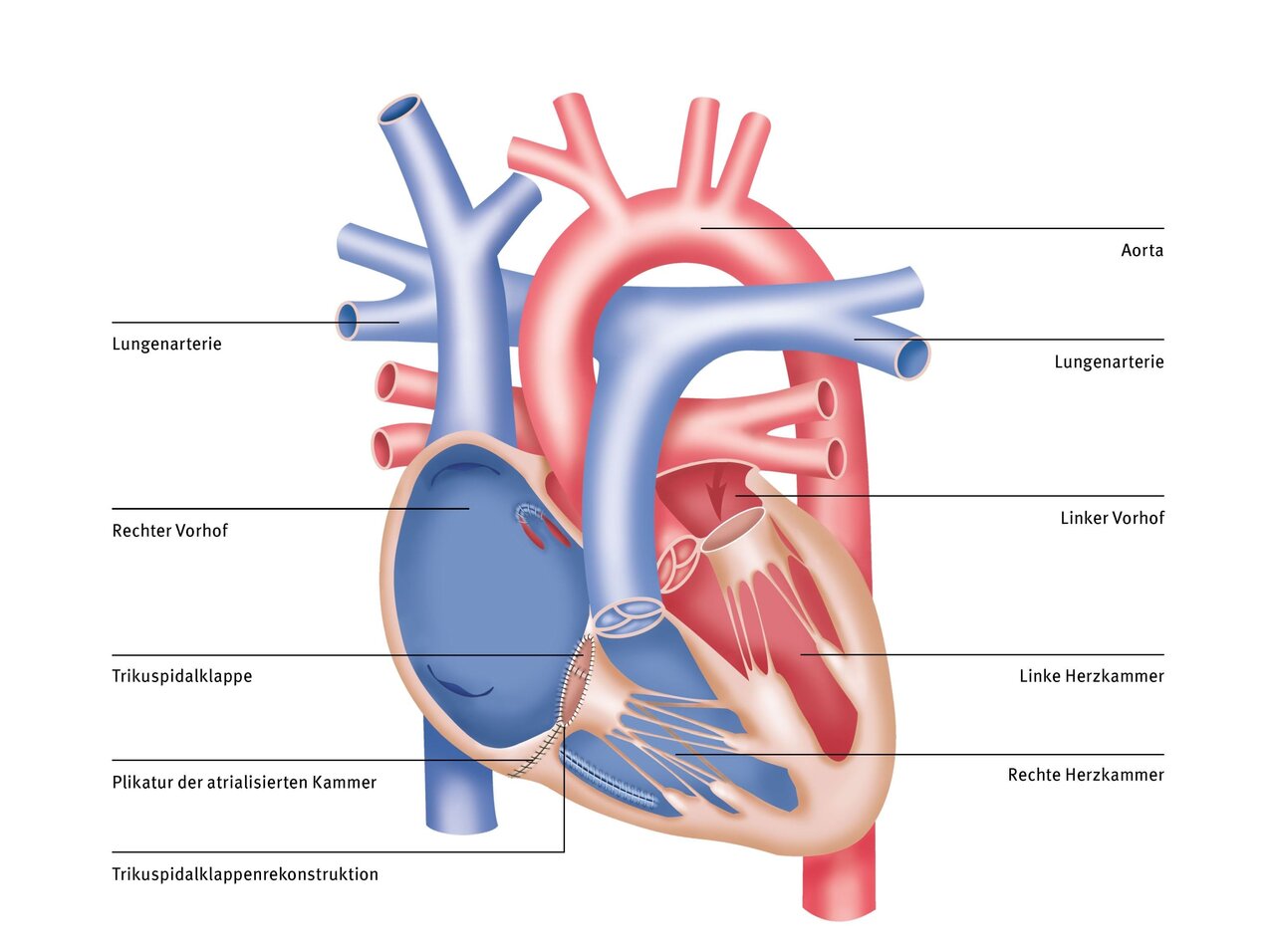
Initially, the disease is treated with medication. If the patient's state of health deteriorates, the tricuspid valve is corrected using a heart-lung machine. The aim of this surgical reconstruction is to restore the function of the tricuspid valve and improve the pumping function of the right ventricle. The doctors at the DHZC use various innovative reconstruction techniques for this purpose. The cone method according to da Silva is favoured. This involves mobilising the valve leaflets and reconstructing them in a funnel shape; the right ventricle is also tightened.
In some cases, however, patients have to have an artificial heart valve implanted. The timing and extent of the operation are determined on an individual basis; in very rare cases, an operation may be necessary in the neonatal period.
We have been using what is known as “fast-track extubation” for many years: after open-heart surgery using a heart-lung machine, we ensure that patients can breathe independently again quickly. This reduces the risk of respiratory infections.
- More about fast-track extubation

Therapy at the DHZC
At the DHZC, we offer Starnes procedures, cone reconstruction, and tricuspid valve replacement. In addition, we offer the fast-track concept for operations such as cone reconstruction or tricuspid valve replacement, whenever possible. This means that your child will be weaned off the ventilator while still in the operating room and will be transferred to the pediatric intensive care unit already breathing independently. In the past, this has contributed to fewer days in the intensive care unit and faster discharge home.
Cardiac catheterization at the DHZC
In two specially equipped and state-of-the-art cardiac catheterization laboratories of the Clinic for Congenital Heart Defects – Pediatric Cardiology examine and treat newborns, infants, children, and adolescents of all ages with congenital and acquired heart diseases, as well as all adults with congenital heart defects. As a supraregional center of excellence, we specialize in invasive cardiological diagnostics and interventional therapy for patients with congenital heart defects. Our team has many years of experience and expertise.
Questions and answers for parents (FAQ)
Your child's ability to exert themselves after the operation depends on the surgical procedure chosen. Even patients with a severe form of Ebstein's anomaly can usually achieve normal everyday exertion levels after the operation. Depending on the severity of the Ebstein's anomaly and the surgical procedure, your child may be advised against competitive sports. Immediately after the operation, it may also be necessary to refrain from strenuous activity for a short period of time until healing is complete. Your pediatric cardiologist will advise you individually on this. Following Starnes surgery, medication is always necessary to prevent blood clots from forming in the shunt.
Depending on the surgical procedure, the pediatric cardiologist should examine your child at specific intervals. After Starnes surgery, more frequent pediatric cardiology checkups are necessary. In addition, a cardiac catheterization and, if necessary, further diagnostics must be performed to determine whether the conditions for circulatory separation or tricuspid valve reconstruction are met.
After successful cone reconstruction, the outlook is good. However, your child will still need regular check-ups with a pediatric cardiologist or, later on, with a cardiologist specializing in adults with congenital heart defects (EMAH) in order to detect any long-term effects, such as atrial arrhythmia or renewed valve leakage, in good time.& nbsp;
After surgery for Ebstein's anomaly, your child will need to take antibiotics as a preventive measure before certain procedures, such as dental work. This procedure is called “endocarditis prophylaxis” and is intended to prevent bacteria that enter the bloodstream during dental procedures from settling in the previously operated heart. Your pediatric cardiologist will inform you individually whether this so-called endocarditis prophylaxis needs to be continued for more than six months.
The outlook in terms of life expectancy and quality of life depends on the severity of the disease. Following successful surgery, 20-year survival rates of over 90 percent can now be expected.
A repeat intervention or operation is always necessary after a Starnes operation, even if the cone reconstruction is successful. After a Starnes operation, a decision must be made as to whether circulatory separation, and thus a circulatory situation with only one ventricle, is the best option. In this case, further cardiac catheter examinations and two additional operations must be performed.
If cone reconstruction is performed, the valve may still leak again later in life, requiring further surgery. The development of atrial arrhythmias such as atrial fibrillation is also common and may require treatment by means of catheter ablation.


