Truncus arteriosus communis (TAC)
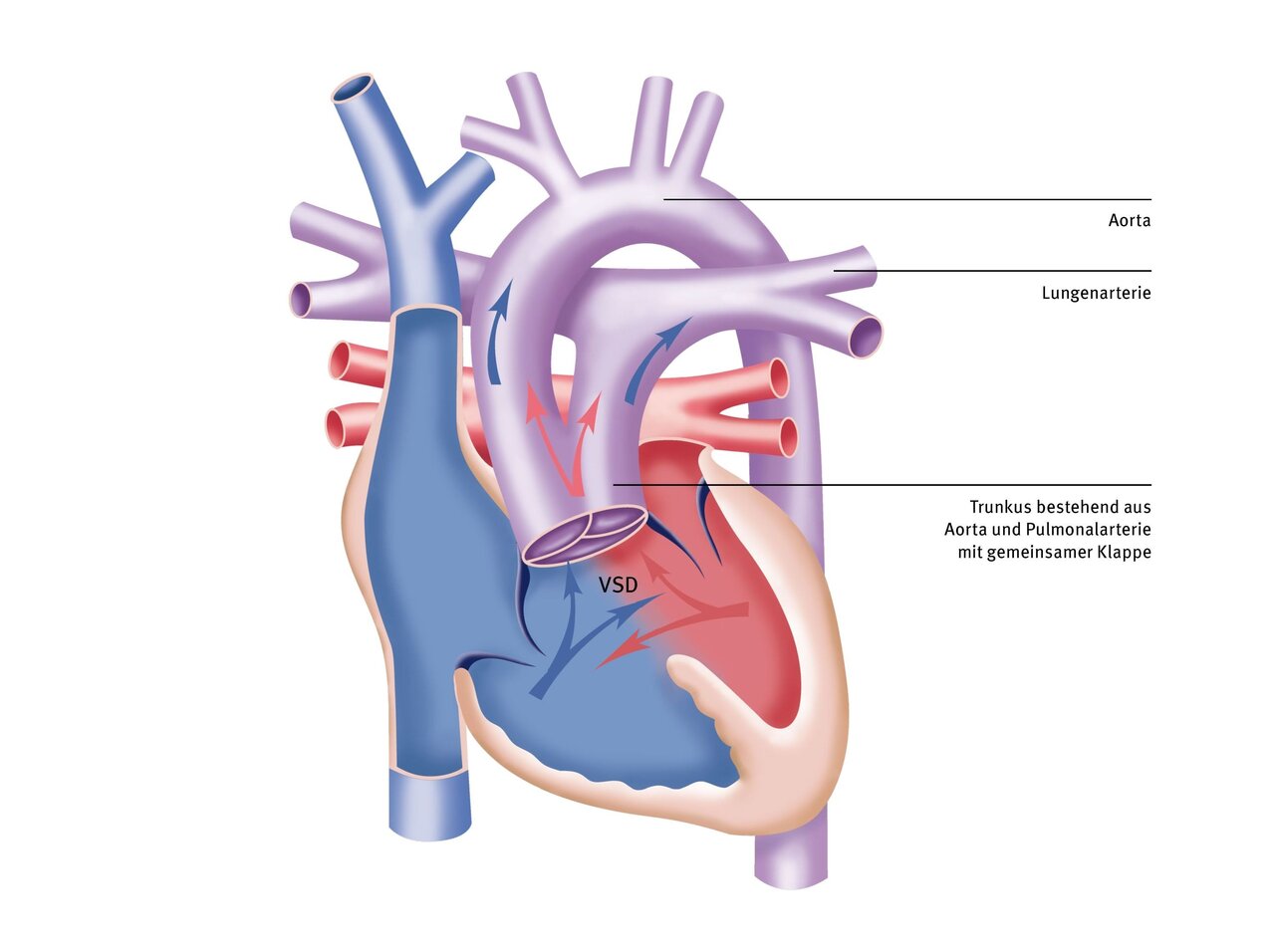
The truncus arteriosus communis (TAC) is a rare congenital heart malformation that accounts for only 0.5 - 0.8% of all heart defects. Its origin is based on a lack of ingrowth of the aortopulmonary septum: in this heart defect, only one artery emerges from the heart (conotruncal malformation).
Both the aorta and the pulmonary artery originate from this main trunk, the so-called ‘truncus’. The ‘truncus’ originates above a ventricular septal defect (VSD), which is always present in this heart defect. This ‘truncus’ then receives both oxygen-poor blood from the right ventricle and oxygen-rich blood from the left ventricle. This mixture of deoxygenated and oxygenated blood is then transported to both the body and the lungs. This heart defect can only be corrected by surgery. TAC is typically diagnosed prenatally by ultrasound and postnatally by echocardiography.
Cause
The exact cause of TAC is unknown. However, there are several risk factors that contribute to the development of this heart defect. These include nicotine consumption by the mother, especially during the first trimester of pregnancy, and folic acid deficiency.
Up to 33 percent of children with a TAC also have what is known as DiGeorge syndrome. This is a genetic defect that occurs when part of chromosome 22, containing genetic information, is lost in the earliest stages of embryonic development.
Symptoms
Initially, the newborns are relatively unremarkable, but after the pulmonary vascular resistance drops, the first clinical symptoms appear in the first few weeks of life. Typically, cardiac insufficiency (accelerated breathing, difficulty drinking and failure to thrive, susceptibility to infection) increases with advancing age. Correction is therefore targeted as early as the second to fourth week of life.
Echocardiography is the most important diagnostic procedure for confirming a TAC. It provides information about the anatomy and function of the heart without requiring invasive measures. This allows, for example, the common arterial trunk and the presence of a ventricular septal defect to be directly detected. The heart valves and heart function can also be assessed using this method.

Diagnosis
- Echocardiography
- Cardiac catheterisation only in exceptional cases
- Additional chromosome analysis if necessary
Many heart surgeries can only be performed on a stopped heart. A heart-lung machine takes over the function of the heart and lungs during surgery.
The DHZC has twelve modern heart-lung machines at its disposal, three of which are specifically designed for infants and young children.

Therapy
The operation
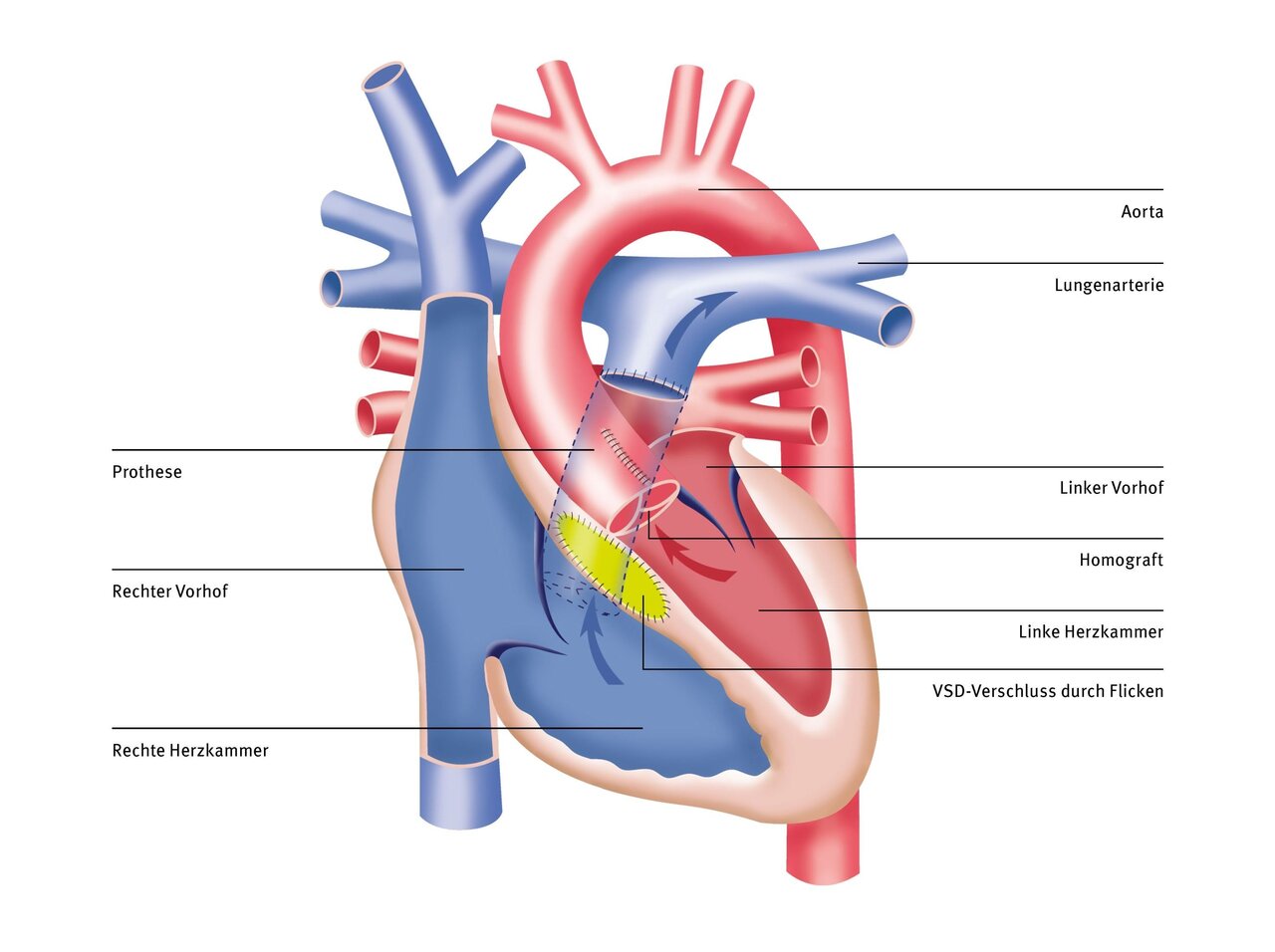
After opening the chest and starting the heart-lung machine, the heart is stopped using a cold infusion solution. The right ventricle is opened and the ventricular septal defect is closed above it. The two pulmonary arteries are then separated from the truncus and connected to the right ventricle with the help of an artificial vessel, a so-called conduit. The aorta is reconstructed with a patch.
The prognosis after the operation is good, but follow-up operations are necessary as the conduit does not grow and degenerates over the course of the patient's life and has to be replaced several times.
Possible complications in the long term
A conduit replacement is usually required within the first five years of the operation. The risk of such a routine repeat procedure is not very high.
Depending on the morphology of the truncal valve, additional stenoses or, much more frequently, insufficiencies may occur, making re-operation necessary.
The overall prognosis is good, endocarditis prophylaxis for the known indications is necessary.
Treatment at the DHZC
At the DHZC, we offer the fast-track concept for operations such as TAC correction, whenever possible. This means that your child will be weaned off the ventilator while still in the operating room and will be able to breathe independently when they are transferred to the pediatric intensive care unit. In the past, this has contributed to shorter stays in the intensive care unit and faster discharge home.
More about pediatric heart surgery at the DHZC
In two specially equipped and state-of-the-art cardiac catheterization laboratories of the Clinic for Congenital Heart Defects – Pediatric Cardiology we examine and treat newborns, infants, children, and adolescents of all ages with congenital and acquired heart diseases, as well as all adults with congenital heart defects. As a supraregional center of excellence, we specialize in invasive cardiological diagnostics and interventional therapy for patients with congenital heart defects. The services we offer include closure of all types of vascular malformations as well as closure of atrial septal defects and ventricular septal defects using implants.
Questions and answers for parents
After a successful TAC repair, your child can usually resume normal physical activity. Immediately after a truncus arteriosus repair, it may be necessary to refrain from strenuous activity for a certain period of time until healing is complete. Some children may need to avoid more strenuous activity. Your pediatric cardiologist will advise you individually on this.
Even after successful primary correction of a TAC, you should have your child undergo regular follow-up examinations with your pediatric cardiologist. During these examinations, special attention should be paid to the blood flow through the neo-aorta and aortic valve as well as the new pulmonary artery.
As with any surgery, complications can occur after the procedure. For example, the truncus valve may leak even after an initially successful corrective surgery. Depending on the type of corrective surgery, the new pulmonary artery may become too narrow. This impedes blood flow to the lungs and forces the right heart to work continuously against increased resistance. If this is the case, the new pulmonary artery must be replaced again.
For a period of around six months after TAC surgery, your child will need to take antibiotics as a preventive measure before certain procedures, such as dental work. This procedure is called “endocarditis prophylaxis” and is intended to prevent bacteria that enter the bloodstream during the procedure from settling in the heart that has undergone surgery. Your pediatric cardiologist will inform you individually whether this so-called endocarditis prophylaxis needs to be continued for more than six months, e.g., if the VSD cannot be closed immediately.
The outlook for life expectancy and quality of life is good after timely TAC correction. In some cases, heart problems may develop in subsequent years even after initially successful correction. These can include progression of pulmonary arterial hypertension or leakage of the operated heart valves. The development of cardiac arrhythmias, which usually only occur in adulthood, is also possible. Long-term survival after successful correction is currently estimated at approximately 80 percent after 30 years.
Even if the corrective surgery is successful, one or two further operations are usually necessary before your child reaches adulthood. The pulmonary artery, which has been reshaped using foreign material, cannot keep pace with your child's physical growth, meaning that your child will “outgrow” their pulmonary artery, which will then need to be widened or replaced. Leaks in the valves can also be addressed in such an operation.
In order to delay surgery, an intervention using a cardiac catheter may also be performed if necessary. If a cardiac arrhythmia occurs in adolescence or adulthood, accompanied by a slow heart rhythm, a pacemaker may need to be implanted. However, this is rather rare.


