Partial anomalous pulmonary venous drainage (PAPVD)
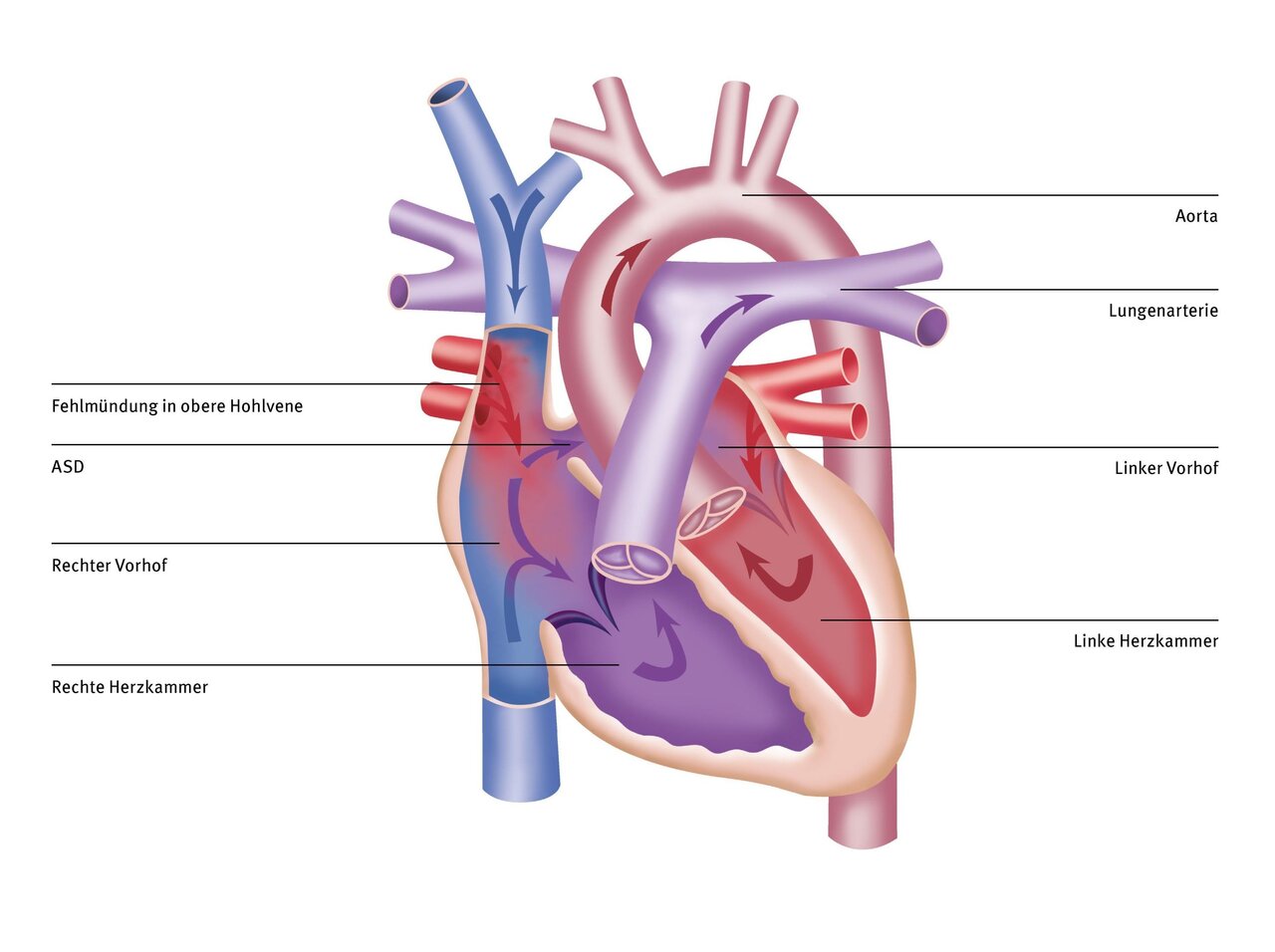
PAPVD, or partial anomalous pulmonary venous drainage, refers to the abnormal drainage of one or more pulmonary veins. The four pulmonary veins transport oxygen-rich blood from the lungs to the left atrium. From there, it enters the left ventricle of the heart and then flows through the aorta into the body.
In PAPVD, one to three of the pulmonary veins drain into another part of the right heart or the large systemic venous vessels. This causes oxygen-poor and oxygen-rich blood to mix. Often there is also a defect in the wall between the right and left atria, known as an ASD (atrial septal defect).
There are different forms of PAPVD. PAPVD can occur alone or in combination with other congenital heart defects.
Cause and effect
The cause of PAPVD is not yet known. PAPVD develops during embryonic development in the womb.
What does this mean for the heart and circulation?
Normally, the pulmonary veins carry oxygen-rich blood from the lungs to the left atrium. A malformation of the pulmonary veins means that the pulmonary veins carry the oxygen-rich blood to the right side of the heart, usually to a large vein or the right atrium. From there, the blood flows back to the lungs.
In summary, the blood circulates between the lungs and the right side of the heart. As a result, less oxygen-rich blood enters the systemic circulation and too much blood flows through the pulmonary circulation.
Symptoms
The symptoms of a child with PAPVD vary depending on the number of veins with abnormal connections. Children with only one missing vein are usually asymptomatic.
If there are several missing veins on the same side and/or an accompanying ASD, your child may experience shortness of breath during exertion or frequent bronchopulmonary infections.
If PAPVD remains untreated into adulthood, excessive blood flow to the pulmonary arteries leads to high blood pressure in the pulmonary arteries (“pulmonary arterial hypertension,” or PAH for short). PAH is difficult to treat and is associated with a significantly reduced life expectancy.
Many heart surgeries can only be performed on a stopped heart. A heart-lung machine takes over the function of the heart and lungs during surgery.
The DHZC has twelve modern heart-lung machines at its disposal, three of which are specifically designed for infants and young children.

Treatment
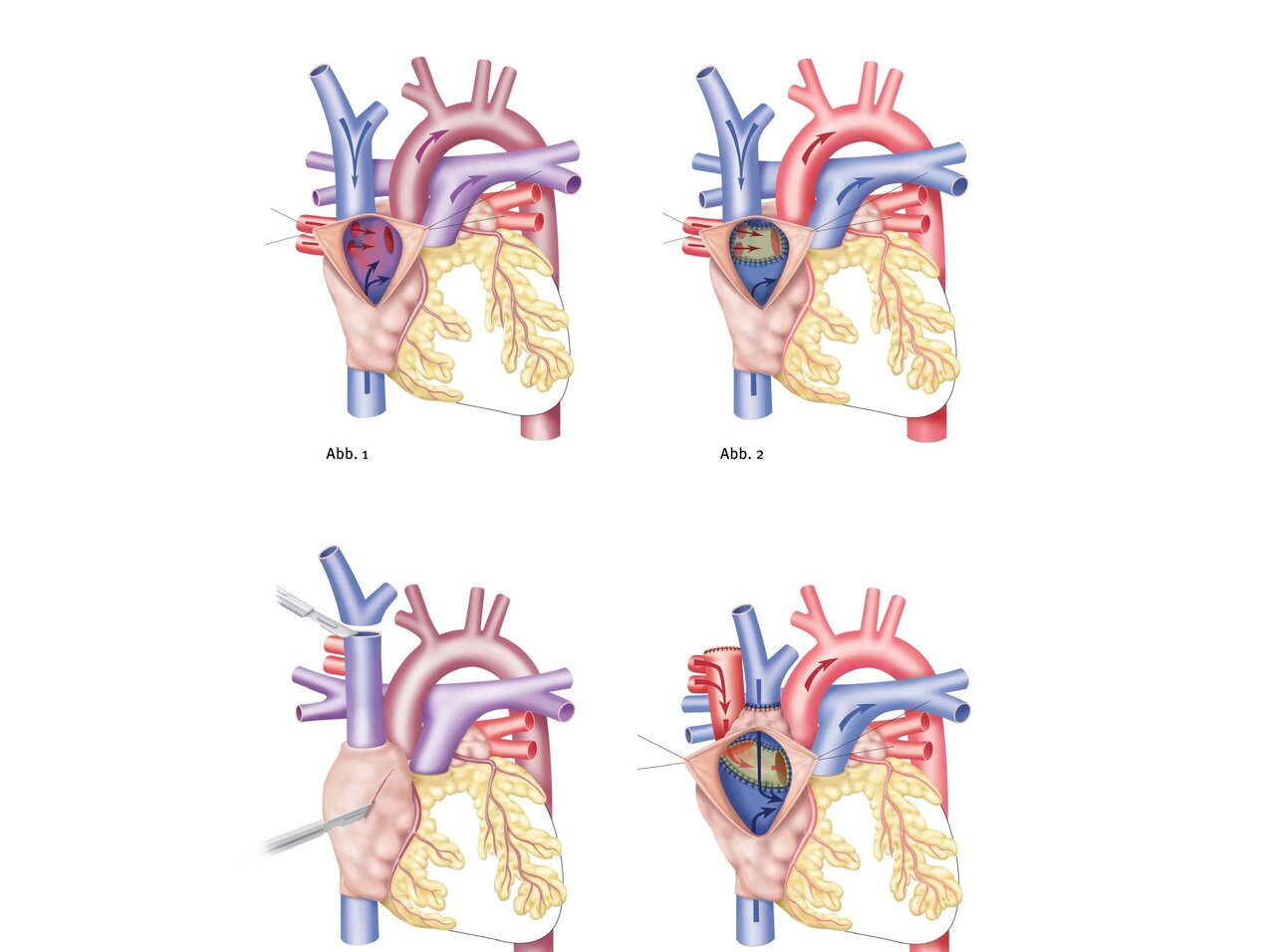
PAPVD must always be corrected surgically by open-heart surgery using a heart-lung machine. Unlike other septal defects, an accompanying ASD in PAPVD cannot close on its own.
There are medications that can support your child's heart until corrective surgery and alleviate the symptoms. However, these medications have no effect on the heart defect and do not protect against high blood pressure in the pulmonary arteries.
During the operation, the misdirected pulmonary veins are redirected to the left atrium using one or two patches. If there is an accompanying ASD, the pulmonary veins are “tunneled” through the ASD into the left atrium. The patch is usually made from the patient's own pericardium, i.e., the outer layer of the pericardial sac in which the heart lies in the chest.
The incision that the pediatric heart surgeon must make during the operation runs vertically between the nipples. In many cases, minimally invasive access is also possible from the right side of the chest between the ribs. Surgical PAPVD correction must always be performed under general anesthesia.
Treatment at the DHZC
At the DHZC, we offer PAPVD correction via a cosmetically advantageous, minimally invasive approach on the right side of the chest for suitable patients. In order to perform surgery using this approach, MRI imaging must first be used to ensure that the malformed pulmonary veins are not too far away from the right atrium. Ideally, MRI imaging should be performed on an outpatient basis several weeks before surgery so that we can plan the ideal access route with you. In many, but not all, cases, this allows us to avoid making an incision in the middle of the chest and cutting through the sternum.
Where possible, we offer the fast-track concept at the DHZC for operations such as PAPVD correction. This means that your child will be weaned off the ventilator while still in the operating room and will be transferred to the pediatric intensive care unit already breathing independently. In the past, this has contributed to shorter stays in the intensive care unit and faster discharge home.
In addition, we examine and treat patients in two specially equipped and state-of-the-art cardiac catheterization laboratories at the Clinic for Congenital Heart Defects – Pediatric Cardiology We treat newborns, infants, children, and adolescents of all ages with congenital and acquired heart diseases, as well as all adults with congenital heart defects. As a supraregional center of excellence, we specialize in invasive cardiological diagnostics and interventional therapy for patients with congenital heart defects.
As a supraregional center of excellence, our cardiac catheterization laboratory at the Clinic for Congenital Heart Defects – Pediatric Cardiology specializes in invasive cardiological diagnostics and interventional therapy for patients with congenital heart defects.

Questions and answers for parents
The outlook for life expectancy and quality of life is very good after timely PAPVD correction.
In rare cases, heart problems may occur in the years following an initially successful correction. These include narrowing of the pulmonary or systemic veins where the corrective surgery was performed. The development of cardiac arrhythmias, which usually only occur in adulthood, is also possible.
After successful PAPVD correction, your child can usually resume normal physical activity. Immediately after PAPVD correction, it may be necessary to refrain from strenuous activity for a short period of time until healing is complete. Some children may need to avoid strenuous activity for longer. Your pediatric cardiologist will advise you individually on this.
Even after successful correction of PAPVD, you should take your child for regular check-ups with your pediatric cardiologist. These check-ups should focus on ensuring unrestricted blood flow through the diverted pulmonary veins and systemic veins. In addition, the heart rhythm should be checked regularly.
A narrowing of the diverted pulmonary veins or systemic veins may necessitate further surgery or cardiac catheterization. For about six months after PAPVD correction, your child will need to take preventive antibiotics for certain procedures, such as dental work. This procedure is called “endocarditis prophylaxis” and is intended to prevent bacteria that enter the bloodstream during dental procedures from settling in the previously operated heart. You should discuss with your pediatric cardiologist whether this endocarditis prophylaxis needs to be continued for more than six months.
Even if the corrective surgery is successful, narrowings may develop in the diverted pulmonary veins or systemic veins over time. This is very rare, but may necessitate further reconstruction through surgery or cardiac catheterization. If a cardiac arrhythmia occurs in adolescence or adulthood that is accompanied by a slow heart rhythm, a pacemaker may need to be implanted. However, this is also rare.


