Heart failure
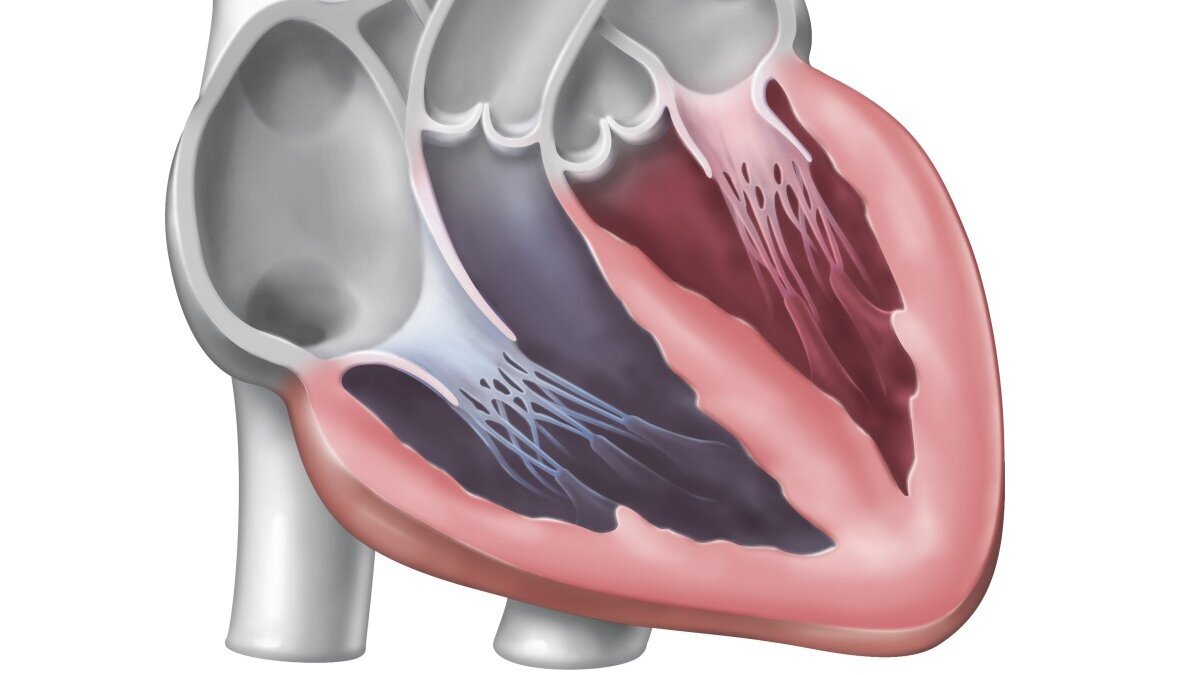
In heart failure (also known as cardiac insufficiency or cardiac insufficiency), the heart is no longer able to supply the body and thus organs such as the brain, muscles or kidneys with sufficient blood and therefore oxygen. The limited pumping capacity of the heart can then lead to typical symptoms such as shortness of breath, fluid retention (oedema) and exercise restrictions.
In Germany, more than four million people suffer from heart failure; the number of sufferers is growing continuously. Heart failure is the most common disease leading to hospitalisation and one of the most frequent causes of death in Germany. Initially, it is often asymptomatic. If heart failure is recognised early and treated in a targeted manner, the progression of the disease can often be slowed down. In this way, the patient's quality of life can be maintained for a long time.
Heart failure
In heart failure, the heart's pumping capacity is restricted. As a result, the heart is no longer able to supply the body and therefore organs such as the brain, muscles or kidneys with sufficient blood and oxygen.
Characteristics
A distinction is currently made between two forms of heart failure, regardless of the cause: if the heart muscle can no longer pump strongly enough, patients suffer from heart failure with reduced ejection fraction (HFrEF). On the other hand, there is heart failure with preserved ejection fraction - heart failure with preserved ejection fraction, HFpEF for short. In this case, the heart pumps normally but is too stiff to fill the ventricles with enough blood.
The ejection fraction is used to estimate the extent of the cardiac impairment. This refers to the percentage of blood volume that is ejected from a ventricle during a cardiac action - in relation to the total volume of the corresponding ventricle. An ejection fraction of more than 55 per cent is considered normal. A severe restriction is defined as an ejection fraction of less than 35 per cent.
Symptoms
Heart failure often begins insidiously and is therefore often not recognised at first. This is because the heart's pumping power only gradually decreases. The first symptoms are non-specific: performance decreases, those affected become exhausted more quickly, feel short of breath and have to take more frequent breaks. Other symptoms include tiredness, low blood pressure and palpitations. Breathing may also be disturbed during sleep. Finally, cardiac pulmonary oedema (‘water in the lungs’) can occur with severe shortness of breath and leakage of fluid into the alveoli.
Causes
Heart failure can have very different causes. The most common cause is calcification of the coronary arteries, known as coronary heart disease. The calcification narrows the vessels that supply the heart muscle; the blood can no longer flow through them properly. As a result, the heart muscle is undersupplied and is less efficient.
Other causes include
- Diseases of the heart valves
- permanent cardiac arrhythmia such as so-called ‘atrial fibrillation’
- congenital or acquired heart valve diseases, e.g. aortic stenosis or mitral valve insufficiency
- Tissue diseases and infections of the heart muscle itself, e.g. cardiomyopathies or myocarditis
- Arterial hypertension (high blood pressure in the arteries)
Telemedical care can prolong the lives of patients with advanced heart failure and lead to fewer hospitalisations.

Risk factors
In addition to these causes, there are other risk factors that favour the progression of heart failure. One decisive aspect for the occurrence of heart failure is age: people over the age of 40 have an increased risk of developing heart failure. The risk increases further with age.
Other risk factors include
- Obesity
- physical inactivity
- Diabetes mellitus
- renal insufficiency
- heavy alcohol consumption
Gender-associated influencing factors
There are known differences between the sexes in the development and progression of heart failure, as well as in the response to treatment and medical care. Both biological sex and gender as a socio-cultural construct (norms, behaviour, role in society) play a role here.
Overall, women suffer less frequently from heart failure than men, even though the risk of developing the disease increases with age in both sexes. The reason: the female sex hormones oestrogens have a protective effect against the development of atherosclerosis, in which the arterial blood vessels become diseased. This disease can lead to heart failure in the long term.
Changes in hormonal balance after the menopause also play an important role in the development of cardiovascular disease, which can cause heart failure.
Social gender potentially influences risk behaviour and lifestyle, use of health care or prevention, disease perception and decision making in relation to therapies.
Electrocardiogram (ECG)
The electrical activity of the heart can be measured using an ECG. The heart action is recorded in the form of curves. The ECG therefore provides reliable information about the health of the heart.
(Image: DHZC)

Diagnosis
The primary diagnosis is made using a combination of clinical examinations, echocardiography and certain laboratory values:
- The NT-Pro-BNP value of the patient can be determined in the laboratory . NT-Pro-BNP (‘N-terminal pro-B-type natriuretic peptide’) is a hormone that is produced and released in the heart when the pressure in the heart increases. An increased NT-Pro-BNP value can indicate heart failure.
- Ultrasound examinations of the heart ( echocardiography): In echocardiography, ultrasound waves are emitted via a so-called transducer and either ‘swallowed’ or reflected back by the body tissue. Ultrasound is used to visualise the heart muscle, the heart valves and the large vessels.
- Electrocardiogram (ECG): The ECG refers to the measurement of the electrical activity of the heart. The heart action is recorded in the form of curves. This provides the doctor with information about the state of health of the heart, as the formation and spread of electrical excitation is altered in many diseases.
- In individual cases, a computerised tomography (CT) or magnetic resonance imaging (MRI) of the heart may be necessary.
- Cardiac catheterisation: A ‘cardiac catheterisation’ is an examination of the heart, in particular the coronary vessels and the heart chambers. Using a thin plastic tube (catheter) and a contrast agent, the doctor can visualise the coronary vessels and the heart chambers on an X-ray screen in order to see any circulatory disorders of the heart or pumping force disorders.
Therapy
At the DHZC, we offer the entire spectrum of modern diagnostic and therapeutic options in cardiology, paediatric cardiology and cardiac surgery. We work together with many clinics and outpatient practices in Berlin and Brandenburg and have set up the Berlin Heart Failure Programme. We also act as a supra-regional heart failure centre for Berlin and have been able to jointly establish cross-institutional interdisciplinary case discussions, common standards for diagnostics and therapy as well as initiatives for the further education and training of medical and nursing staff. The aim is to set new standards in the field of heart failure treatment.
All modern cardiovascular diagnostic and therapeutic procedures are available at our clinic (including MRI, CT, electrophysiology, cardiac catheterisation for the treatment of coronary vessels and heart valves, pacemaker implantation, surgical procedures including bypass surgery, valve surgery, mechanical circulatory support and heart transplantation).
Artificial hearts
We offer mechanical circulatory support systems for circulatory support. A distinction is made between short-term and long-term systems.
In short-term systems, the actual pump is located outside the body. Heart and lung functions are supported in the short term to prevent the brain from being undersupplied. Pump systems supply the body with blood, relieve the heart and support blood circulation. Patients with these systems can be mobilised, but are dependent on the hospital.
If the heart is unable to recover or recovery takes longer, ventricular assist devices - i.e. long-term systems - are used. These ‘artificial heart systems’ consist of a small pump that the surgeon inserts directly into the patient's heart. Most patients with an artificial heart can lead a largely normal life. More than half of them are on the waiting list for a donor heart. With over 3,400 artificial heart implantations to date, the DHZC, under the direction of Prof. Evgenij Potapov, operates the largest artificial heart programme in the world.
Artificial hearts
Long-term support systems, so-called artificial hearts, are used when the heart is unable to recover.

Heart Failure Centre of the DHZC
The Deutsches Herzzentrum der Charité is Berlin's supra-regional heart failure centre. It is certified according to the criteria of the German Society of Cardiology (DGK). In our outpatient clinic for severe heart failure and cardiomyopathies and on our certified heart failure ward , we specialise in the diagnosis and treatment of heart failure. We treat both patients with common causes (e.g. dilated cardiomyopathy, severe myocardial infarction) and those with more unusual diagnoses (e.g. storage diseases or inflammatory heart muscle diseases including cardiac amyloidosis and myocarditis).
Our services are tailored to the individual patient's situation. We treat both patients who have been diagnosed with heart failure or cardiomyopathy for the first time and who have not yet received cardiological care, as well as patients who have been suffering from heart disease for a long time and are receiving appropriate cardiological treatment. If their state of health deteriorates despite treatment, we examine further therapeutic options such as catheter-based and surgical options. We also initiate special treatment methods for patients with severe heart disease - including mechanical circulatory support or organ transplantation.
In addition to the DHZC and Charité, the specialists at both centres have launched the Berlin Heart Failure Programme (BeHIP) . BeHIP has set itself the goal of improving the care of patients with heart failure in Berlin and the surrounding area together with other clinics and practices through a series of measures. These include the networking of outpatient and inpatient healthcare facilities, the organisation of further education and training events for both doctors and nurses (e.g. for heart failure nurses) as well as training for patients and their relatives.
In addition, the Transsectoral Heart Failure Network Berlin Southwest Brandenburg provides comprehensive care for patients with chronic heart failure together with specialist cardiological practices and GPs in the region and offers free training courses to provide valuable information on how to deal with their disease in everyday life. The network is based at the Department of Cardiology, Angiology and Intensive Care Medicine at the Benjamin Franklin Campus. Contact persons are Prof Dr Bettina Heidecker (Senior Physician and Head of the Heart Failure and Cardiomyopathy Clinic at the CBF) and certified heart failure nurse Daniela Hinrichs.
Heart failure self-check
Do you suffer from heart failure? Our heart failure self-check (only available in German) will help you manage the condition.

Cardiac exercise for heart failure
Patients who suffer from heart failure can generally do sport. It is important that they consult their doctor in advance. Sports that are suitable for patients with heart failure include walking or cycling. However, heart failure patients should refrain from exercise if they have an acute infection, chest pain, shortness of breath or dizziness.
Cardiac exercise is a suitable rehabilitation measure to accompany cardiological treatment. It can significantly improve patients' physical and mental performance. It is important that a doctor is always present in addition to the exercise instructor. Cardiac exercise is prescribed by a doctor and subsidised by health insurance companies. The DHZC offers cardiac exercise for patients with severe heart failure and patients with artificial heart systems as part of a study. Training takes place once a week in small groups of a maximum of 7 people. The training includes gymnastics and coordination exercises, endurance training and relaxation exercises.
Cardiac exercise
At the DHZC, patients with heart failure can train once a week in small groups. The training programme includes gymnastics and coordination exercises, endurance training and relaxation exercises.
(Image: DHZC)




