Parent information
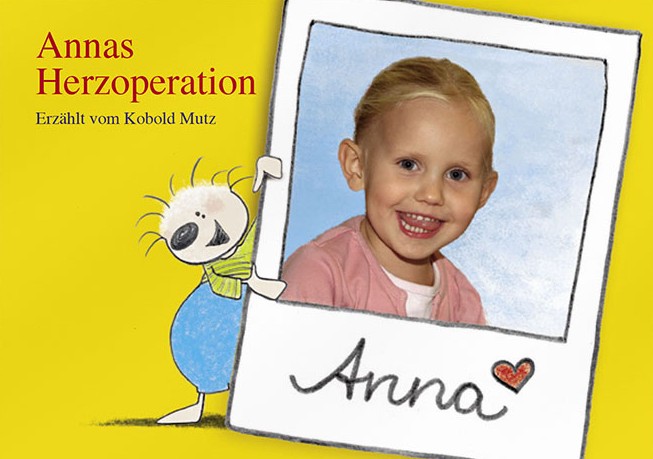
Our interactive children's book with diary accompanies younger children and their families before heart surgery. The little goblin Mutz looks after little Anna during her stay in hospital.
As part of this, we try to explain every step of the treatment to you as clearly as possible during a premedication interview – the necessary preparations for the operation, what will happen in the operating room, the measures required to monitor you and the further care after the operation. We take time for you and your questions.
The premedication interview takes place during our anesthesia consultation hours on ward WD2 or in your room. During this personal conversation between the anesthetist and the patient, the medical history, including current medication, is recorded and all findings are evaluated. Knowledge of previous illnesses and current medication is important for the anesthetist to administer a safe and comfortable anesthesia.
The anesthetic procedure used depends to a large extent on the planned surgery. However, as far as the procedure allows, patient preferences will of course be taken into account.
We will also inform you about the necessary procedures before the operation, for example, to what extent fasting is required or whether you should continue taking any medication you are already on.
During the conversation, you can and should discuss your questions, but also any fears and concerns you may have regarding the anesthesia with our team, so that we can explain everything to you as precisely as possible.
To ensure that the procedures in our anesthesia consultation run smoothly, we ask that you complete the anesthesia questionnaire given to you on the ward in advance, if possible. Please also bring your current medication plan and, if available, an allergy pass, emergency pass or anesthesia ID card.
It is our aim to help you return to your normal daily routine as quickly as possible.
Our competent team of doctors and nurses is at your disposal around the clock with extensive experience, contemporary anesthesiological concepts and procedures, and the help of the latest medical technology. Our highly qualified specialists are specially trained to care for patients undergoing heart surgery, continuously update their knowledge in this field, and in turn ensure that their colleagues receive future-oriented further training.
All of the department's medical staff have undergone special training in transesophageal echocardiography (a swallowing ultrasound examination of the heart) and are always on hand to support their surgical and interventional colleagues with their expertise. In cardiac surgery in particular, the activities of the anesthesiology and surgery departments are interlinked like gears in a machine. At the German Heart Institute Berlin, we see ourselves as one team with a common goal: your health.
The word “anesthesia” comes from ancient Greek and means “insensitivity”. In medicine, it refers to the elimination of certain sensory qualities, in particular the sensation of pain and touch. Not every form of anesthesia necessarily leads to loss of consciousness.
While conventional heart surgery involving opening the chest and using a heart-lung machine is normally performed under general anesthesia, catheter-based procedures such as interventional aortic valve replacement aortic valve or the MitraClip procedure for the treatment of mitral valve insufficiency can also be performed under local anesthesia or in a painless twilight sleep, a so-called analgosedation.
For most operations and procedures, we need vascular access to monitor your cardiovascular functions and to control your therapy. These are small, thin plastic tubes that are placed securely and painlessly in blood vessels using ultrasound, primarily in the wrists, on the side of the neck or in the groin. This is done either under local anesthesia or, if a general anesthetic is planned, only after induction of the anesthetic sleep. Of course, we continuously monitor the depth of your anesthesia during all general anesthetics, so that intraoperative wakefulness or an excessively deep level of anesthesia are extremely unlikely.
Regardless of the procedure chosen, the rapid restoration of your ability to function is particularly important to us. That is why a large proportion of the procedures we perform are designed from the outset to be fast-track. These procedures combine less invasive surgical techniques and particularly short-acting anesthetic methods to ensure an even faster recovery and convalescence.
You are in good hands with us.
That is why we have a nursing and medical team at the German Heart Center of the Charité that is specially trained in this area.
All anesthetists in our pediatric cardiac anesthesia department are board-certified anesthesiologists with extensive experience in cardiac surgery, certification in cardiac ultrasound (echocardiography), and often additional qualifications in specialized intensive care, emergency medicine, and/or pediatric echocardiography, to name just a few. It is important to us that you know your child is in good hands.
In the run-up to the operation, we will discuss all the details of the anesthesia and anesthetic measures with you in detail and answer all your questions precisely and comprehensibly.
We are happy for parents to accompany their child to the entrance of the operating wing on the day of surgery. However, it is not possible for them to accompany their child into the operating room or induction room. In addition, the understandable nervousness and emotional tension of parents and accompanying persons often unintentionally transfers to the young patient. We ask for your trust and understanding that it is not possible for you to be present during the operation.
One of the fundamental principles in anesthesiology is that the extent of monitoring measures depends on the severity of the patient's underlying illness and the complexity of the planned procedure. Monitoring cardiovascular function is, of course, a central aspect of cardiac surgery. Safety is our top priority. This means, for example, that in our young patients, various vascular catheters (including the so-called central venous catheter, or CVC for short) are placed under ultrasound guidance for blood pressure monitoring and for the administration of drugs and fluids close to the heart, even before the operation begins, but already under anesthesia. In addition, a bladder catheter is usually inserted to monitor kidney function. In addition, we continuously monitor brain function and blood flow during all procedures using highly sensitive electrodes and sensors attached to the skin.
Another important component of the anesthetic measures for monitoring and diagnosing our youngest patients is transesophageal echocardiography (TEE/TOE). Depending on the size of the child, an ultrasound probe, which is sometimes tiny, is inserted into the oesophagus, similar to an endoscope used in a gastroscopy. Since the heart is anatomically located directly next to the oesophagus, the pediatric anaesthetists and pediatric cardiologists obtain images of the heart and its function in the highest quality, which guide the surgical and drug therapy.
Complex corrective procedures often take time. Nevertheless, it is sometimes advantageous and, for certain types of surgery, even proven to be more beneficial to wake the young patient quickly after the end of the procedure and to remove the breathing tube – of course accompanied by a well-thought-out pain management program adapted to the child's needs. The team at the Clinic for Cardioanaesthesiology and Intensive Care Medicine and our colleagues at the Clinic for Surgery of Congenital Heart Defects have been working together on this so-called fast-track principle for some time, examining it for suitable procedures and investigating the possible advantages. We can therefore look back on extensive and positive experience with this procedure. In joint discussions, we determine the best course of action for each patient individually.
After cardiac surgery, patients are cared for in the pediatric intensive care unit of the German Heart Institute Berlin, where the colleagues from the Clinic for Congenital Heart Defects – Pediatric Cardiology take over further care. After a detailed handover and a report on the surgical procedure and anesthesia, your child will receive intensive care here until transfer to the general ward. The detailed monitoring and any necessary circulatory and pain therapy will, of course, continue seamlessly.
You can rely on our professionalism and care.
For a more child-friendly illustration of a hospital stay involving heart surgery, we recommend, for example, the book “Annas Herzoperation” (Anna's Heart Operation), which is available online from the Bundesverband Herzkranke Kinder e. V. (German Federal Association for Children with Heart Disease). You can access it via the following link:
https://bvhk.de/wp-content/uploads/2016/11/Annas-Herzoperation-deutsch-Download.pdf
The recovery room is a separate area of the operating room where you or your relatives wake up quickly and stress-free from the anesthesia, are quickly weaned from ventilation and thus regain full independence as early as possible.
The PACU is an important interface between the operating room, the intensive care unit and the so-called normal wards: every day, we take over patients from the entire spectrum of heart surgery directly from the operating room, who, according to the criteria of our fast-track protocol, can wake up from anesthesia within a very short time after the operation.
This concept has proven particularly successful at the German Heart Center of the Charité for operations performed as so-called “minimally invasive surgery” (MIS) (e.g. MIS mitral valve reconstruction/replacement, MIS aortic valve replacement, minimally invasive bypass surgery). These patients are usually already awake and responsive within the first few hours after the procedure, can be mobilized early and recover quickly. After treatment in the PACU has been completed, further care in an intensive care unit is usually only necessary until the next day.
If you are undergoing a catheter-based interventional procedure (including TAVI, Mitra-ClipTM, endovascular procedures such as TEVAR/EVAR) or, for example, a pacemaker implantation or revision, you will need adequate postoperative care in a specialized monitoring unit , where circulation, heart rhythm, breathing, bleeding tendency, laboratory values, etc. are monitored, controlled and, if necessary, treated. However, you do not have to be treated overnight in an intensive care unit; if you are stable, you can be transferred back from the PACU to the normal ward during the course of the day of the operation.
Intensive care
After many heart surgeries, more intensive monitoring and therapy is necessary. This takes place in the intensive care units 1 or 2 at the German Heart Institute Berlin. After many heart surgeries, more intensive monitoring and therapy is necessary. This takes place in the intensive care units WD1I, W1I and WD2I at the DHZC.
You will usually still be under anesthesia when you are taken from the operating room to the intensive care unit, so you will not remember the first few hours. After admission, the anesthesia is ended and as soon as you wake up and your breathing has sufficiently recovered, the breathing tube (trachea) can be removed. The continuous administration of medication, which may have been necessary during the operation to stabilize heart function and blood pressure, can often also be stopped over the next few hours. You may be able to drink again or even have a light meal on the evening of the operation.
Every surgical procedure is associated with pain. These are eliminated by the anesthetic during the operation. In the intensive care unit, you will continue to receive medication so that you will wake up largely free of pain. After that, we will continue to closely monitor the dose of pain medication you need to actively contribute to your recovery. Our goal is for you to be sitting at the edge of your bed with the help of physiotherapists and eating breakfast independently the morning after surgery, so that you can be transferred to the post-operative care ward on the first day after surgery.
Occasionally, the so-called weaning from artificial ventilation also takes a few days. This is particularly the case with pre-existing lung conditions or heart failure. In these cases, we will give you medication that will enable you to tolerate the breathing tube in your windpipe. Even under these circumstances, our goal is to keep you awake, for example, to prevent muscle weakening through physiotherapy.
In addition, continued administration of medications to support circulation or other organ dysfunction, such as acute renal failure, may be reasons for a longer period of treatment in the intensive care unit.
After certain surgeries, such as transplants, insertion of a left or right ventricular assist device (LVAD/RVAD) or emergency surgeries, a longer ICU stay is also to be expected. On each of these treatment days, a highly specialized and motivated team of experienced nurses, physical and respiratory therapists, and medical staff will work with you to help you achieve your personal health and independence goals as quickly as possible.
Acute brain dysfunction may occasionally occur, especially after heart surgery. This condition, known as delirium, is characterized by acute confusion and behavior that is inappropriate to the situation, possibly self-endangering, as well as abrupt changes in wakefulness.
To reduce the likelihood of you experiencing delirium, various measures have been introduced at the DHZC. These include, among other things, the avoidance of excessively deep anesthesia by measuring brain waves (EEG), avoiding sedation (“artificial coma”) in the intensive care unit if possible, and a documented reorientation after the operation. For this purpose, you will receive your glasses and hearing aid back on the day of surgery, should you require them. Your relatives can also contribute to your recovery and reorientation by visiting you in the intensive care unit: they can explain to you where you are, what has happened and what is being done to help you recover, or what is happening in your familiar environment. It also often helps if you have a picture of importance to you in sight or are given books and current magazines during longer treatment periods.
Various medical devices are necessary in an intensive care unit to monitor and, if necessary, support organ functions. These can be intimidating for patients and/or relatives, so we would like to introduce you to the most important ones below:
Monitors are usually placed both next to and above the patient's bed. They constantly display the cardiac electrical activity (EKG), blood pressure, oxygen content of the red blood cells (oxygen saturation) and body temperature. Other measurements can also be displayed if needed.
Arterial catheters are often placed to enable accurate measurement of blood pressure. These are thin tubes that are placed in an artery in the wrist or groin.
Syringe pumps continuously inject medication into the blood. This may include medication to support the cardiovascular system (catecholamines), to fight infections (antibiotics) or even pain medication. Central venous catheters (CVCs) are often required for this. These are thin tubes that are inserted into a large blood vessel in the neck or under the collarbone.
Ventilation equipment is available if you are still unable to breathe sufficiently on your own or if your lungs have not yet fully recovered. With the help of a breathing tube (tracheostomy tube) inserted through the mouth into the windpipe or a mask, the ventilator can deliver an oxygen-air mixture to the lungs to support breathing.
Even if you are unable to speak through the breathing tube, we will always enable you to communicate directly with the treatment team and your relatives. This can be as simple as answering yes/no questions by moving your head or eyes. Alternatively, writing tablets or electronic devices (tablets, smartphones) can also be used.
As long as you are unable to eat normally, nutrition will be administered via a tube leading through the nose into the stomach (gastric tube) or, in rare cases, via the central venous catheter.
A urine catheter was inserted through the urethra into the bladder during the operation. This allows urine to drain continuously and the urine production to be measured. The urine catheter itself can, however, lead to a feeling of urgency, which quickly subsides.
In the rare case of severe cardiac and/or pulmonary dysfunction, miniaturized heart-lung machines (ECMO; extracorporeal membrane oxygenation) are available. These can use pumps to extract blood from the body via larger catheters, enrich it with oxygen and then return it to the body.
Audible and visible alarms provide information about even the smallest changes in the monitored bodily functions. As a rule, an alarm is intended to draw attention to a specific situation so that appropriate measures can be taken. Only in the rarest of cases does it indicate a threatening situation. So an alarm does not have to make you feel insecure.
Intensive care treatment still relies on equipment. However, the focus of our therapy is always on you and your individual needs, as well as the involvement of your relatives. Our goal is for you to regain your strength as quickly as possible so that you can leave our ward.

Don't be afraid of pain!
Often, the idea of having an operation is associated with a fear of pain after the operation or even with painful previous experiences of this kind. However, good pain management is essential for a speedy recovery and early mobilization. Pain relief begins with the introduction of anesthesia and is continued intra- and postoperatively. In the first hours after surgery, painkillers are administered intravenously in the intensive care unit or PACU by the medical staff caring for you. As soon as you are awake and responsive, you will receive pain management according to a proven pain management plan developed in-house that is tailored to your individual needs.
As a rule, a combination of different painkillers is used, which are taken regularly according to a schedule. In addition, you can receive further painkillers as needed.
In order to be able to adjust the need for painkillers precisely, you will be asked to estimate the severity of your pain using a pain scale. This pain measurement is carried out by the nursing staff or during the doctor's rounds and to check the effect of painkillers. This pain measurement/pain assessment determines the pain at rest and in motion. Movement such as getting up or coughing often has the effect of intensifying pain, especially after surgery. An important goal of pain management is to avoid relieving posture and to achieve early mobilization.
To be honest, it must be noted that in the first postoperative days - especially if drains are still in the surgical area - complete freedom from pain (corresponding to a value of 0 on the scale below) often cannot be achieved.
Therefore, or despite this: don't be afraid of pain!
The realistically achievable value on the pain scale with appropriate pain therapy is 2 to 3; from a value of 4, there is a need for intervention.
Please be sure to let us know if you are in pain!
Only you can judge your pain, and your perception of pain is our benchmark, which we address individually. To do this, we will ask you to rate the intensity of your pain on a scale from 0 to 10, where 0 means no pain and 10 corresponds to the strongest imaginable pain.
While no one can guarantee absolute freedom from pain after an operation, we are only satisfied when you are.
