Cardiovascular arrest
Cardiac arrest is the third most common cause of death in Europe. Cardiovascular arrest occurs when the heart suddenly stops beating. This means that the heart is no longer pumping blood through the body. Without this blood circulation, the organs, including the brain, can no longer receive oxygen, which can very quickly become life-threatening. If help is not given immediately, this can lead to death within minutes. Current surveys show that the chances of survival after a cardiovascular arrest have improved in recent years.
Differentiation
Cardiac arrest can occur both in and out of hospital. Accordingly, it is referred to as an ‘in-hospital’ or ‘pre-hospital’ cardiac arrest.
In special cases, there is a so-called ‘refractory cardiovascular arrest’. Refractory cardiac arrest is a form of cardiac arrest in which standard resuscitation measures are not successful in restoring sustained spontaneous circulation after a set period of time, typically 15 minutes. Extended resuscitation measures can be considered for selected patients.
Symptoms
The symptoms of cardiac arrest are often very clear and include
Unconsciousness: the affected person does not respond to speech or touch.
Respiratory arrest or ‘paradoxical’ breathing: The person is not breathing or is breathing irregularly and/or with gasping breaths.
If one of the above two criteria is present, the emergency services should be alerted immediately and resuscitation measures carried out. It is important to act quickly if these symptoms are noticed, as every minute counts. Immediate action can save lives.
There are also other symptoms, but you should not spend too much time investigating them.
Absence of pulse: No palpable pulse, especially in the large arteries (neck or wrist).
Pale or bluish skin colour: The skin may be pale or bluish in colour, especially on the lips and fingernails.
No response to stimuli: No response to painful stimuli (such as pinching).
Dilated pupils: Pupils may be dilated and no longer sensitive to light.
First aid
Rapid and accurate diagnosis of a cardiac arrest is crucial in order to initiate the right treatment and increase the chances of survival for the person affected. A ‘rescue chain’ describes the sequence of actions taken in an emergency to help a person quickly and effectively. Here are the steps in simple terms:
- Secure and make an emergency call
- Provide first aid
- Rescue service takes over
- Hospital treatment
These steps work together to ensure that the person concerned gets the best possible help.
ToDo: Warnhinweis "Ersthelfer/112" / Bild ERC / Link zu Erste Hilfe Kursen (?)
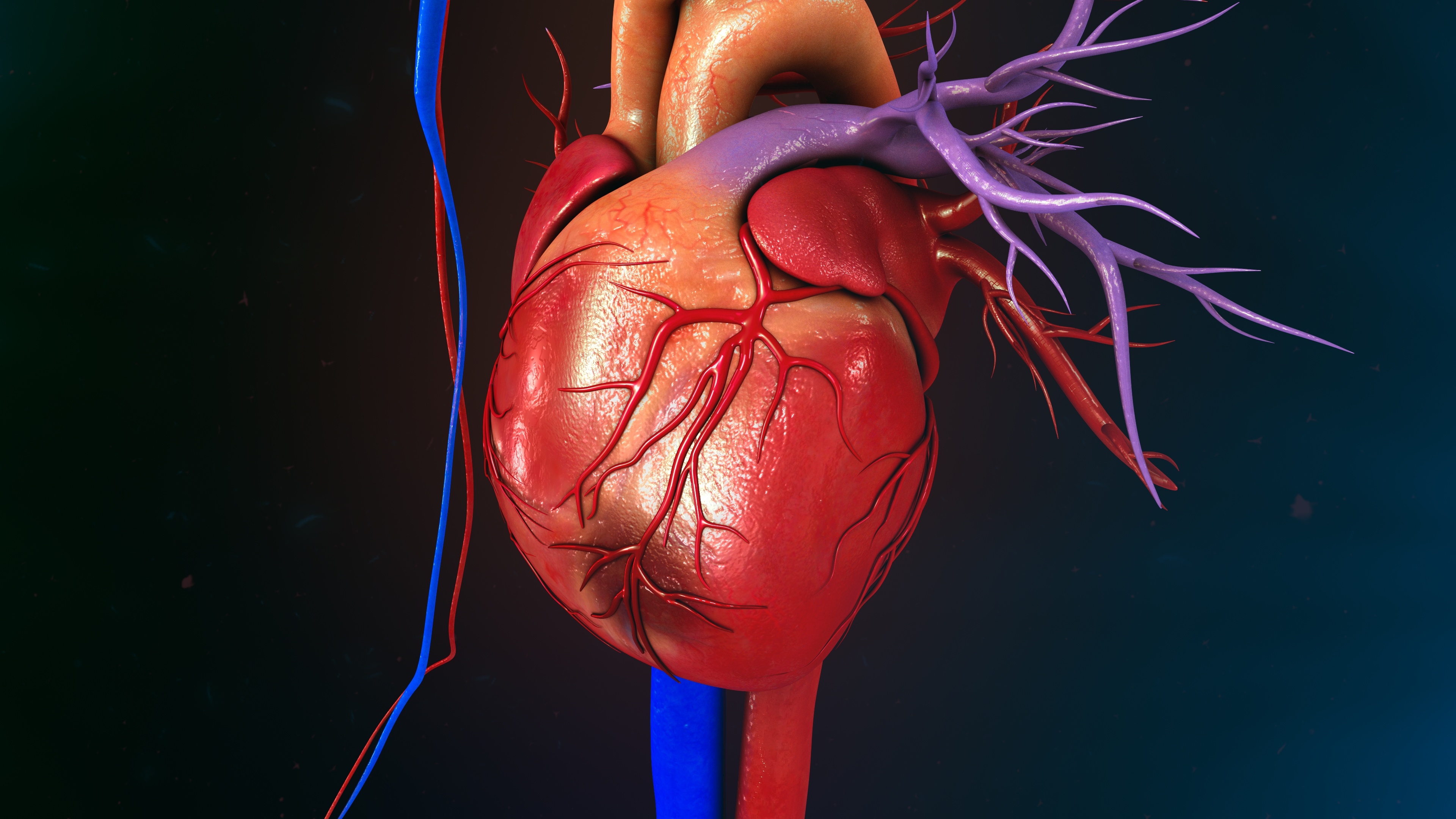
One of the most common causes of cardiovascular arrest is a heart attack.
However, cardiac arrhythmias, heart failure and diseases of the heart muscle or heart valves are also among the cardiovascular diseases that can trigger a cardiac arrest.
Causes
Cardiac arrest can be triggered by various causes. Here are some of the most common:
- Heart attack (‘acute myocardial infarction’): One of the most common causes. A heart attack occurs when the blood supply to part of the heart is blocked, resulting in damage to the heart muscle.
- Heart rhythm disturbances (‘arrhythmias’): Abnormal heart rhythms, such as ‘ventricular fibrillation’ or ‘ventricular tachycardia’, can cause the heart to stop pumping effectively.
- Heart failure (‘cardiac insufficiency’): When the heart is no longer able to pump enough blood due to conditions such as ‘cardiomyopathy’ or severe valvular heart disease.
- Heart muscle disease (‘cardiomyopathies’): Diseases of the heart muscle that affect the heart's ability to pump blood.
- Heart valve diseases (‘valvular heart disease’): Severe problems with the heart valves can affect the flow of blood through the heart.
- Respiratory arrest (‘apnoea’): Problems with breathing, such as choking, severe asthma attacks or a blocked airway, can lead to cardiac arrest.
- Electrical accidents: An ‘electrical shock’ can throw the heart out of rhythm and cause cardiac arrest.
- Trauma: Severe injuries, especially to the chest, can directly damage the heart.
- Drowning: A lack of oxygen due to drowning can lead to cardiac arrest.
- Drug overdose (‘intoxication’): Certain drugs, especially those that affect the heart or breathing, can cause cardiac arrest.
- Severe infections (‘sepsis’): Sepsis can lead to multiple organ failure, including the heart.
- Severe haemorrhage: Major blood loss can cause the heart to not have enough blood to pump.
These causes show that cardiovascular arrest is often the end result of several serious health problems. Rapid intervention is crucial to increase the chances of survival.
Risk factors
here are several risk factors that can increase the likelihood of cardiovascular arrest. These factors can include both medical conditions and lifestyle factors:
- Pre-existing heart conditions:
- Coronary artery disease (CAD): narrowing of the coronary arteries due to calcium deposits.
- History of heart attack: Increases the risk of further heart problems.
- Cardiac arrhythmia: Abnormal heart rhythms such as atrial fibrillation or ‘ventricular tachycardia’.
- Heart failure: A weak heart that does not pump enough blood.
- Heart valve disease: Leaky or narrowed heart valves.
- Family history: A family history of heart disease or sudden cardiac death.
- High blood pressure (hypertension): Increases pressure on the heart and blood vessels.
- High cholesterol: Can lead to deposits in the arteries that reduce blood flow to the heart muscle.
- Diabetes: Increases the risk of heart disease and cardiovascular arrest.
- Smoking: Damages the blood vessels and increases the risk of heart disease.
- Obesity: Increases the risk of high blood pressure, diabetes and heart disease.
- Lack of exercise: It can lead to weight gain, high blood pressure and high cholesterol.
- Unhealthy diet: A diet rich in saturated fats, trans fats, salt and sugar can increase the risk.
- Alcohol and drug abuse: It can directly damage the heart and increase the risk of arrhythmia and heart disease.
- Stress: Chronic stress can contribute to high blood pressure and other heart problems.
- Age: The risk increases with age.
- Gender: Men have a higher risk of cardiac arrest than women, especially at a younger age.
- Electrolyte imbalances: Imbalances in electrolytes such as potassium or magnesium can lead to cardiac arrhythmias.
The combination of several risk factors increases the overall risk of cardiovascular arrest. Preventive measures such as regular medical check-ups, a healthy lifestyle and the management of existing health problems can help to reduce the risk.
Diagnosis and therapy
The diagnosis and treatment of cardiac arrest are closely linked, as rapid action is crucial:
- Initial assessment at the scene of the emergency:
- Consciousness check: Check whether the person is responding to speech or touch.
- Breathing assessment: Check that the person is breathing normally. This can be done by observing chest movements or listening and feeling for breathing.
- Emergency measures:
- Make an emergency call: Call 911 immediately and request professional help.
- Cardiopulmonary resuscitation: Immediately perform chest compressions and ventilations at a ratio of 30 compressions to two breaths if no breathing or pulse is detected.
- Use of an automated external defibrillator (AED):
- Analysing heart rhythms: An AED automatically analyses the heart rhythm and, if necessary, delivers an electric shock to bring the heart back into a normal rhythm.
- Advanced medical diagnostics in hospital or by the emergency services
- Continuous cardiopulmonary resuscitation: Continuation of cardiopulmonary resuscitation by professional rescuers (if necessary with the aid of mechanical resuscitation aids) until spontaneous circulation returns or until further measures can be taken.
- Drug treatment: Administration of drugs such as adrenaline and amiodarone to support the heart and stabilise the rhythm.
- Defibrillation: Regular heart rhythm analyses are carried out and, if necessary, shocks are delivered using a defibrillator.
- Advanced airway management: Intubation or other methods to ensure breathing and oxygenation.
- Imaging procedures: An ultrasound scan is performed specifically on the heart, lungs, abdomen and pelvis.
- If spontaneous circulation can be restored, various diagnostic and therapeutic agents are used:
- Electrocardiogram (ECG): An ECG is performed to monitor cardiac activity and detect abnormal rhythms.
- Blood tests: Checking blood values, e.g. for electrolytes, cardiac markers or markers of infection, which may indicate a possible cause.
- Imaging procedures: X-rays,echocardiography, computed tomography or other imaging techniques may be used to identify structural problems.
- Cardiac catheterisation: If a heart attack is suspected, a cardiac catheterisation may be performed to identify and treat blocked coronary arteries.
Special moulds
Refractory cardiac arrest describes a condition in which cardiac arrest persists for a prolonged period of time despite the application of standard resuscitation measures and the circulation does not stabilise.
ECPR
In the case of refractory cardiac arrest,extracorporealcardiopulmonaryresuscitation( ECPR ) can be used as an advanced resuscitation technique in selected patients if conventional resuscitation measures are unsuccessful.
ECMO
It involves the use of a so-called ‘extracorporeal membrane oxygenation device’ (‘ECMO’), which temporarily takes over the functions of the heart and lungs in order to supply the body with oxygen and maintain blood circulation. Suitable candidates for ECPR are often younger patients with immediately initiated resuscitation after an observed cardiac arrest and certain heart rhythms. In patients with severe irreversible pre-existing conditions (e.g. terminal cancer), advanced age and/or poor prognostic factors as well as a long period without oxygen supply (‘hypoxic brain damage’), the use of ECMO should be scrutinised more critically.
During ECMO, large cannulas are inserted into an artery and a vein of the patient (usually in the groin). The blood is channelled out of the body via these cannulas, enriched with oxygen by a so-called ‘oxygenator’ and then returned to the body. The oxygenator takes over the function of the lungs by enriching the blood with oxygen and removing carbon dioxide. The pump of the ECMO device takes over the function of the heart by circulating the blood through the body. While the patient is connected to ECMO, intensive care measures are taken to diagnose and treat the cause of the cardiac arrest (e.g. cardiac catheterisation in the event of a heart attack).
ECMO therefore makes it possible to maintain vital functions while the underlying cause of the cardiac arrest is treated. In suitable patients, ECPR can improve survival rates and neurological outcomes. However, the risks of haemorrhage, reduced blood flow to the legs, infection and vascular injury are increased with ECMO. ECMO patients also require blood thinners, which further increase the risk of bleeding.
Current studies show that ECMO in combination with a miniaturised heart pump (‘Impella®’) could further improve survival in refractory cardiovascular arrest due to a heart attack.
ECPR is a complex and resource-intensive procedure that is carried out in specialised centres with experience in the use of ECMO. In selected cases, it offers an additional chance of survival in otherwise hopeless situations.
Aftercare
Already during and after the monitoring and treatment of affected patients in the cardiological intensive care unit to stabilise the patient, the aim is rehabilitation, i.e. measures to restore health and prevent further cardiac events, including physical therapy, speech therapy and lifestyle adjustments.
For the first time, a ‘resuscitation outpatient clinic’ has been set up at the Benjamin Franklin Campus in collaboration with the Departments of Cardiology, Neurology, Psychology and Sociology, where survivors of cardiac arrest can be followed up.



