Aortic valve stenosis and aortic valve insufficiency
Congenital aortic valve stenosis is a narrowing of the aortic valve caused by incomplete opening of the valve pockets, a valve ring that is too small, or a combination of both.
Aortic valve insufficiency is a leak in the aortic valve, which is usually caused by an impaired closing function of the valve pockets.
A defective aortic valve can either be reconstructed or surgically replaced (Ross operation).
Cause
Congenital aortic valve stenosis accounts for around 3.6 % of all heart defects. In 15-20% of patients, congenital aortic valve stenosis occurs with additional malformations of the heart. The bicuspid aortic valve (only two functioning pockets) is one of the most common valve malformations, which manifests itself in childhood primarily with a reduced opening, and in adolescents and adults often with insufficiency of the valve. It has an incidence of 1-2% in the normal population. In the context of congenital heart defects, the bicuspid aortic valve occurs as an isolated lesion in 61% of cases, otherwise it is frequently associated with other left heart obstructions.
Aortic valve insufficiency can also develop secondary to balloon dilatation or surgery on a primarily stenotic valve, and the severity can increase in the course of the procedure. Rarely, both dysfunctions (stenosis/insufficiency) can develop as part of an infection of the valve (endocarditis) or as a result of an inflammatory autoimmune reaction of the body (rheumatic fever).
Indication
Aortic valve stenosis
If the aortic valve does not open fully or the valve ring is too small (stenosis), the left ventricle has to fight against an unnecessarily high resistance with every heartbeat. In order to be able to do this extra work, the mass of the heart muscle increases steadily. At some point, the system tips out of balance and the mass of the muscle can no longer be adequately supplied with oxygen-rich blood by the existing coronary vessels. The inner layer of the muscle suffers from a lack of oxygen and the heart muscle loses strength and endurance. Symptoms such as palpitations, tachycardia, fatigue, shortness of breath or unconsciousness can occur, especially under stress. Cardiac arrhythmia can also occur.
Aortic valve insufficiency
A disturbance in the closing function of the aortic valve (insufficiency) leads to a permanent overload of the left ventricle with blood volume, which unnecessarily flows back into the heart instead of into the body at the end of each heartbeat. The ventricle becomes larger and larger in order to absorb this volume and to increase the heart rate. If the threshold for this compensation is exceeded, the ventricle can no longer effectively eject the additional volume into the body. This volume is then lacking, especially under stress, in order to supply the muscles and organs with oxygen-rich blood. This results in symptoms such as fatigue, lack of energy, palpitations and failure to thrive.
Symptoms
Depending on the predominant mechanism of valve dysfunction, the severity of the effect on the circulation and the strain on the body, symptoms may occur sooner or later, including heart failure and sudden cardiac death.
Newborns born with severe (critical) aortic valve stenosis are already in a critical condition shortly after birth and require urgent intervention. The burden placed on the heart by the severely stenotic valve must be relieved immediately before heart failure with organ damage occurs. However, most patients have a milder form and only become conspicuous later in life. As a rule, lifelong observation of the findings and symptoms is necessary.
If there are indications of severe stenosis or insufficiency, lack of development or reduced resilience, a step-by-step approach is usually initiated. Measures such as drug treatment, balloon dilation of the valve by cardiac catheterisation and even valve surgery can be combined in order to preserve the function of the left ventricle for as long as possible. A definitive replacement of the aortic valve may be necessary.
Treatment
Surgical procedures on the aortic valve are open-heart operations. This means that the patient is connected to the heart-lung machine and the heart must be immobilised for the procedure in order to operate on the heart valve.
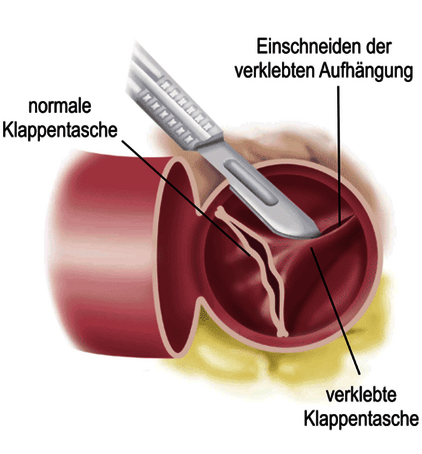
Balloon dilatation/ surgical valvuloplasty
In critically ill newborns and infants, the first option may be to widen (dilate) the valve using a balloon via a cardiac catheter in order to acutely stabilise the circulation and allow the heart function to recover. If the anatomy of the valve pockets is favourable and the circulatory situation is stable, an operation on the aortic valve can be very effective. As a rule, the aortic valve is loosened at the adhered areas and the thickened pockets are thinned out with the aid of a heart-lung machine. With these options, it is usually possible to stabilise the patient and monitor the findings over the course of their life. If the load on the heart should increase again, new interventions must be carried out, which can often only be resolved for a long time with a surgical valve replacement.
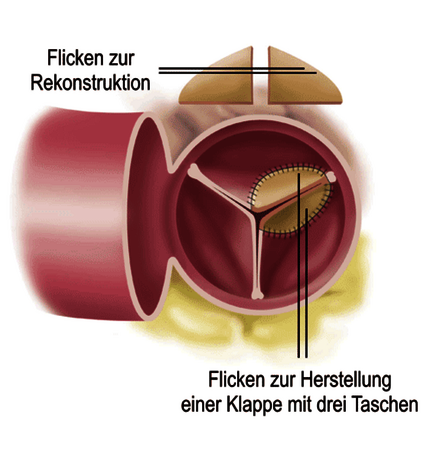
Aortic valve reconstruction
Whenever possible, valve-preserving surgical techniques are used. Aortic valve reconstruction involves reconstructing the incorrectly positioned parts of the valve and replacing the individual pockets with patch material. The durability of such reconstruction procedures is influenced by the individual valve anatomy, the technique used and the accompanying risk factors such as age, previous valve surgery or complex heart defects.
Aortic valve replacement
If valve function can only be restored by valve replacement, there are several options in childhood and young adulthood. Biological valve replacement procedures (valves of human or animal origin) have the advantage that long-term treatment with blood-thinning medication is not necessary. However, with the exception of the Ross operation (replacement with the patient's own pulmonary artery valve), biological valve replacement only has a limited shelf life. As a rule, such valves have to be surgically replaced again in young patients after around five to ten years. A mechanical valve replacement requires a strict lifelong intake of blood-thinning medication with a not inconsiderable risk of bleeding and the formation of blood clots on the heart valve in the long term. Such clots can impair the function of the heart valve or lead to strokes. Any type of valve replacement with a prosthesis (biological/mechanical) has the disadvantage of a lack of growth potential, meaning that these options can only be used sensibly once the patient has reached adult size.
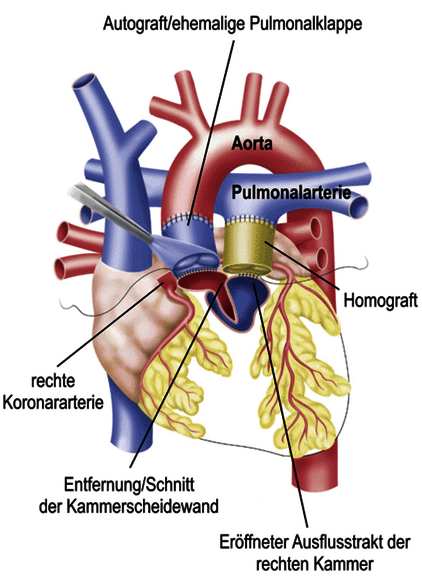
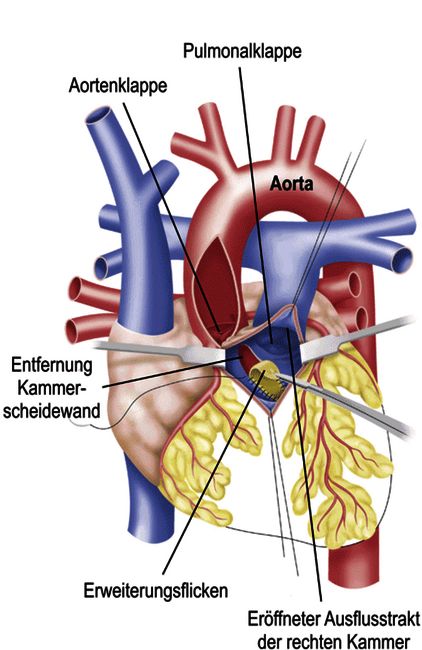
Ross operation
In the Ross operation, the defective aortic valve is replaced by the patient's own pulmonary artery valve (pulmonary valve). As this is the body's own valve, it is also known as an autograft. The pulmonary artery valve is removed and sutured into position after the defective aortic valve has been removed, with or without repositioning the coronary arteries, depending on the surgical technique. The patient's own pulmonary valve is usually replaced with a biological prosthesis. The advantage of this complex operation, especially in children and young adults, is that the new aortic valve (autograft) grows with the patient. The use of strong blood-thinning medication can also be avoided. One disadvantage is the limited durability of the replaced pulmonary valve (usually 10-15 years for biological prostheses) and the late reinterventions on the new aortic valve (autograft). Depending on preoperative risk factors, the patient's age and the surgical technique used, the autograft may fail after around ten years, resulting in a leaky heart valve. In this case, a complex reconstruction of the autograft (e.g. David's operation) or replacement of the entire aortic root may be necessary.
Treatment at the DHZC
The routine use of our heart-lung machine with the world's smallest filling volume makes it possible in the majority of cases - even for newborns - to perform an operation without a foreign blood transfusion, which has considerable advantages. This not only allows us to minimise the risk of infection and intolerance, but often also enables our little patients to recover more quickly after the operation.
The Ross operation is offered in a unique modification of implanting the autograft without detaching the coronary arteries (subcoronary implantation). In this case, the autograft is supported from the outside by the preserved wall of the aorta. This is intended to prevent, or at least delay, the late widening of the autograft and the frequent re-interventions.
Questions and answers for parents
Your child can usually exercise normally after the operation. No restrictions are necessary.
Regular and lifelong check-ups by a doctor specialising in the treatment of patients with congenital heart defects are required. Depending on the surgical method used and any residual findings, medication may be necessary on discharge in individual cases.
Long-term results show that normal development can usually be expected. Exercise tolerance can be normal in patients with mild to moderate findings. Static sports and competitive sports should be avoided for patients with moderate to moderate stenosis.
Depending on the severity of the findings, life expectancy may be shortened, primarily due to the complications of heart failure, the need for repeated reoperations and the risk of cardiac arrhythmia.
When mechanical prostheses are used, the reduction in quality of life can be considerable due to frequent check-ups, increased risk of injury and lifelong anticoagulation. The occurrence of thromboembolic complications (clot formation and risk of stroke) after mechanical aortic valve replacement in children is 0.5 -1 % per patient year.
Freedom from repeat aortic valve surgery has been described after both balloon dilatation by cardiac catheterisation and surgical reconstruction of the aortic valve in the long-term course at around 40% after ten years, while after Ross surgery in the same period 90% of patients still do not require a second procedure. The autograft after Ross surgery shows good adaptation to the child's growth over an observation period of more than eight years. However, the smaller the valve prosthesis used, the greater the need for an intervention in the area of the simultaneously replaced pulmonary valve and this affects younger children more than adolescents or young adults.