Atrial fibrillation is the most common cardiac arrhythmia worldwide. Our heart's pacemaker, the sinus node, normally controls our regular heartbeat. Extra beats from the pulmonary veins can cause the atria to fibrillate, resulting in atrial fibrillation.
In atrial fibrillation, uncontrolled electrical impulses occur in the atria. As a result, the atria can no longer contract rhythmically, but move chaotically: they fibrillate.
Our DHZC information video provides an easy-to-understand overview of cardiac arrhythmias in general and atrial fibrillation in particular. Atrial fibrillation is by far the most common cardiac arrhythmia.
Der normale Herzschlag
Die Pumpfunktion des Herzmuskels wird durch elektrische Impulse ausgelöst und reguliert, die von speziellen Herzmuskelzellen erzeugt und weitergeleitet werden.
Der Sinusknoten im rechten Herzvorhof ist der Taktgeber des Herzens. Hier werden elektrische Impulse erzeugt, im Ruhezustand rund 60 bis 80 mal pro Minute, bei Aufregung oder körperlicher Anstrengung entsprechend häufiger. Die Erregung breitet sich anschließend über die Herzmuskelfasern der beiden Herzvorhöfe aus und bewirkt so deren rhythmische Kontraktion und Entspannung.
Die Grenze zwischen den Herzvorhöfen und den Hauptkammern besteht zu großen Teilen aus Bindegewebe, das die elektrischen Impulse nicht weiterleiten kann und daher als Barriere für die Reizleitung wirkt. Die Impulse treten durch den sogenannten Atrioventrikulären Knoten, kurz AV-Knoten, auf die Hauptkammern über. Diese zweite Bündelung von leitfähigen Herzmuskelzellen ist damit die elektrische Verbindung zwischen den Vorhöfen und Herzkammern.
Der AV-Knoten hat zudem eine Art Filterfunktion: Er bremst bei zu hohen Herzfrequenzen die Erregungsgeschwindigkeit und schützt damit die Hauptkammern vor einer zu hohen Herzfrequenz.
Differentiation of atrial fibrillation
Paroxysmal (attack-like) atrial fibrillation is when the heart returns to a normal rhythm by itself or with the help of an intervention within seven days.
Persistent atrial fibrillation is an irregular rhythm that lasts longer than seven days. This form of atrial fibrillation does not return to a normal sinus rhythm on its own and must be brought back to a normal sinus rhythm with medication or an electric shock.
Long-term persistent atrial fibrillation is when the heart has been in an irregular rhythm for more than 12 months.
Permanent atrial fibrillation is when the atrial fibrillation persists indefinitely and the patient and doctor have decided to stop trying to restore a sinus rhythm.
Risk factors
It is important to note that the presence of one or more of the following risk factors increases the risk of atrial fibrillation, but does not necessarily lead to atrial fibrillation. In general, a healthy lifestyle, good control of blood pressure and other conditions, and regular medical check-ups can help reduce the risk.
Age
The risk of atrial fibrillation increases with age. Atrial fibrillation occurs more frequently in people over the age of 60.
High blood pressure
High blood pressure is a significant risk factor for atrial fibrillation. Permanently high blood pressure puts a strain on the heart and increases the risk of cardiac arrhythmia.
Heart diseases
Certain heart diseases such as coronary heart disease (narrowing of the coronary arteries), valvular heart disease, cardiac insufficiency or congenital heart defects can increase the risk of atrial fibrillation.
Overweight or alcohol
Being overweight or obese puts a strain on the heart and increases the risk of atrial fibrillation. The success of treatment is also reduced in overweight patients. Excessive alcohol consumption can increase the risk of atrial fibrillation.
Sleep apnoea syndrome
Sleep apnoea syndrome is an important risk factor for atrial fibrillation. Sleep apnoea syndrome should definitely be investigated in patients with atrial fibrillation and known breathing interruptions at night. This is also crucial for the treatment of atrial fibrillation.
Symptoms
Patients with atrial fibrillation have very different symptoms, sometimes only very mild symptoms or no symptoms at all. The following symptoms can be caused by atrial fibrillation:
Palpitations, palpitations or irregular heartbeat: Some people describe a rapid, irregular or fluttering sensation in the chest. It can feel as if the heart is out of rhythm.
Reduced exercise tolerance: People with atrial fibrillation may notice a reduction in exercise tolerance. Climbing stairs becomes more strenuous, sometimes even normal everyday activities are no longer manageable.
Shortness of breath: Shortness of breath or the feeling of not getting enough air can occur, especially during physical exertion or at night.
Dizziness or light-headedness: Some people experience dizziness, light-headedness or the feeling of losing consciousness.
Chest pain: Atrial fibrillation can cause chest pain or discomfort in some cases.
It is important to realise that these symptoms can also occur with other conditions. It is therefore essential to consult a doctor to obtain an accurate diagnosis.
Diagnosis
The electrocardiogram (ECG)
An ECG is necessary for the diagnosis of atrial fibrillation.ECG stands for electrocardiogram and refers to the measurement of the electrical activity of the heart.The ECG is a simple examination to perform.This so-called heart action is recorded in the ECG in the form of curves - the famous ‘ECG wave’. This provides the doctor with information about the state of health of the heart, as the formation and spread of electrical excitation is altered in many diseases. In atrial fibrillation, the ECG shows the atrial fibrillation waves and the typical irregular conduction to the ventricle.
Long-term ECG
In some patients, cardiac arrhythmias only occur occasionally. In these cases, a long-term ECG measurement is necessary for a clear diagnosis. An ECG device, which the patient wears on a belt, records the electrocardiogram over a period of 24 to 72 hours. Electrodes are attached to the patient's skin for this purpose.
For rare arrhythmias that cannot be recorded during long-term measurements, we offer recording with a so-called ‘loop recorder’ at the DHZC. With an external loop recorder, the device is worn on a belt and the ECG is recorded via adhesive electrodes attached to the skin.
The measurement is triggered by the patient by pressing a button as soon as an arrhythmia is detected. The implantable ‘Loop Recorder’, on the other hand, is inserted under the skin at chest level. It can record the heart rhythm for up to three years.
Therapy
The most appropriate therapy is decided on an individual basis, taking into account concomitant illnesses, structural changes to the heart and the patient's level of suffering.
If you have been diagnosed with atrial fibrillation, precise therapy planning is required. We know that atrial fibrillation often leads to hospitalisation and the development of heart failure. Current studies show that early effective treatment of atrial fibrillation even improves survival. In principle, the treatment of atrial fibrillation is based on three pillars:
- The need for blood-thinning therapy
- Therapy to maintain the rhythm
- Adjustment of risk factors
Need for blood-thinning therapy
Patients over the age of 65 or patients with risk factors such as high blood pressure or diabetes mellitus as well as patients who have already had a heart failure or a stroke require blood thinning, as atrial fibrillation can cause strokes. You can find out more about the risk of stroke with atrial fibrillation here.
The blood thinner is taken as a tablet and is generally very well tolerated. This also increases the tendency to bleed, so bruising or sometimes nosebleeds can occur more easily. Severe bleeding is rare.
Rhythm maintenance therapy
Rhythm maintenance refers to the therapy that maintains the normal rhythm, i.e. the sinus rhythm, and prevents atrial fibrillation from recurring. There are medications for this that are individually adjusted to the patient. The most effective therapy to date for maintaining sinus rhythm is catheter ablation. Catheter ablation is an interventional, minimally invasive procedure that has been carried out via the groin for over 20 years and is performed under a sleep anaesthetic. It has been proven that atrial fibrillation is caused by extra beats from the pulmonary veins. This is why catheter ablation of atrial fibrillation is also known as pulmonary vein isolation or PVI for short.
PVI requires an inpatient stay with an overnight stay. Sometimes patients also require a second or, more rarely, a third ablation in order to maintain sinus rhythm.
The technology has developed rapidly in recent years. As a university heart centre, all new technologies are available at the DHZC and the procedure is individually tailored to the patient.
Radiofrequency catheter ablation
In catheter ablation with high-frequency current, energy is delivered point by point to the tissue at the opening of the pulmonary veins via the catheter tip. The catheter can be positioned with millimetre precision using X-ray fluoroscopy and a 3D image of the treatment area.
The high-frequency current and the resulting heat cause the cells to lose their electrical conductivity - the pathological impulses can no longer be transmitted to the atrium. The heart beats regularly again.
Pulsed Field Ablation (PFA)
The DHZC is one of the few clinics to offer pulsed field ablation. This ablation treatment takes less time, causes fewer complications and may require fewer follow-up procedures.
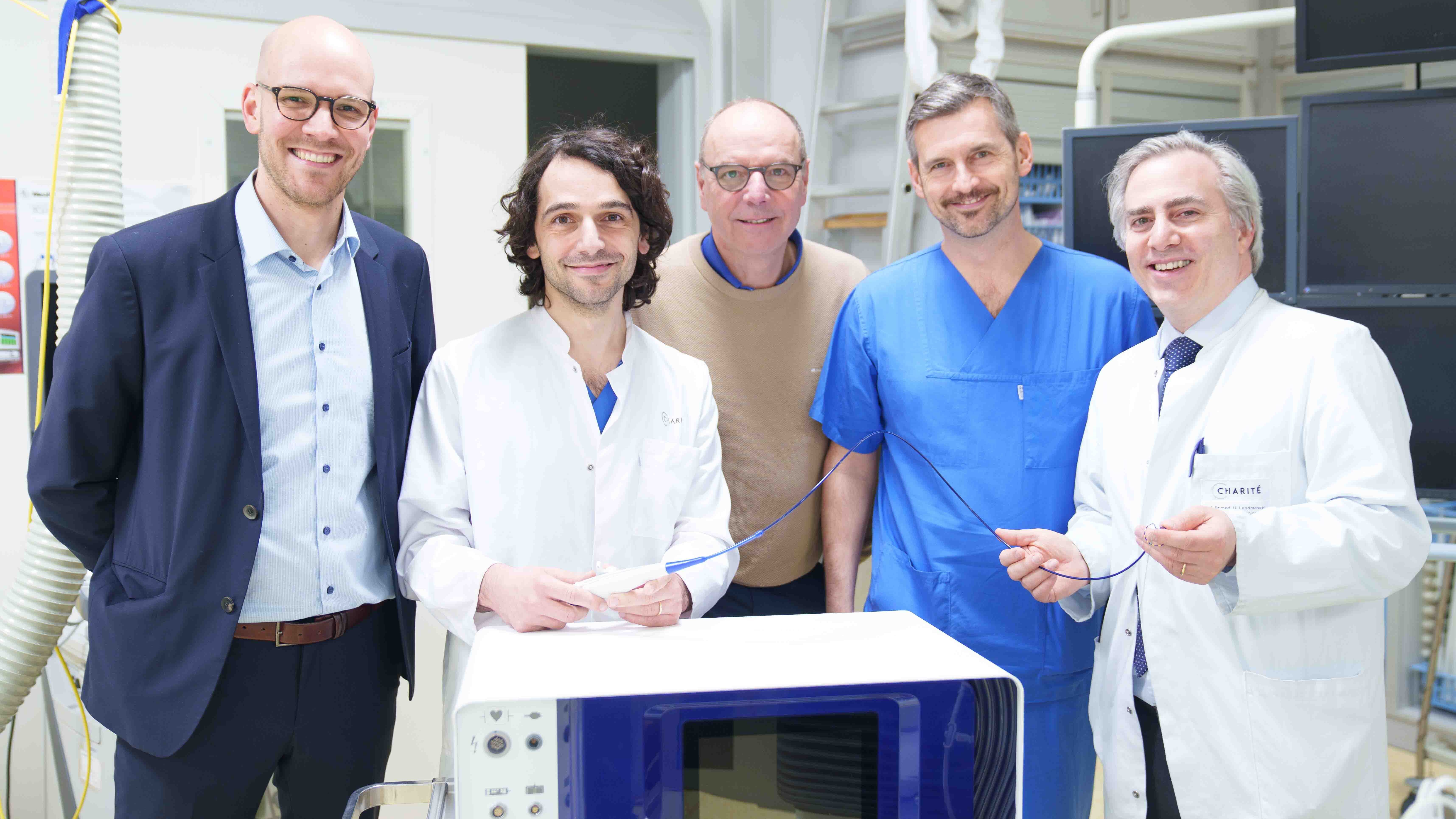
The picture shows members of the DHZC treatment team with a PulseSelect ablation catheter (Photo: DHZC).
- Mehr Informationen
Cryoablation
Another procedure is cryoablation. In this procedure, intense cold is used to stop the pathological conduction. A balloon is usually used for this. This is pushed into the left atrium as far as the mouth of the pulmonary veins and deployed there. The pulmonary veins are sealed tightly with the balloon. The balloon is cooled and the cooling has the effect that the electrical conductivity is no longer transmitted from the pulmonary veins to the atrium and therefore atrial fibrillation can no longer occur.
Pulsed field ablation
The latest technology is pulsed field ablation. It is a very gentle form of ablation. By creating an electric field, only heart muscle cells are attacked. The surrounding tissue, such as the oesophagus or nerve tissue, is completely spared. Current studies have shown hardly any complications affecting the surrounding tissue. The effectiveness in terms of the success rate for treating atrial fibrillation is equivalent to other procedures. This form of ablation is only offered in a few centres in Germany.
Adjustment of risk factors
An important pillar of atrial fibrillation therapy is the treatment of risk factors that patients can significantly influence with their lifestyle.
Prevention of atrial fibrillation
Healthy lifestyle
A healthy lifestyle can reduce the risk of atrial fibrillation. This includes regular physical activity, a balanced diet, sufficient sleep and refraining from smoking. Healthy weight loss and weight control through regular exercise and a healthy diet can reduce the risk. It is recommended that alcohol consumption be moderated or avoided altogether to reduce the risk. This not only reduces the risk of atrial fibrillation, but also increases the success of catheter ablation.
Blood pressure control
High blood pressure is a significant risk factor for atrial fibrillation. Controlling blood pressure through a healthy diet, physical activity and, if necessary, antihypertensive medication can help to reduce the risk.
Control of underlying diseases
Certain underlying conditions such as high blood pressure, diabetes or thyroid disease increase the risk of atrial fibrillation. Good control and treatment of these conditions is important to minimise the risk
Sleep apnoea
Diagnosis and treatment of sleep apnoea also improves the success rate of catheter ablation. If you snore at night and/or have breathing interruptions, talk to your GP about this. Screening for sleep apnoea is easy to carry out.
"We use gentle and innovative procedures to provide optimal care for patients with atrial fibrillation.
We work across clinics and disciplines and have state-of-the-art cardiac catheterisation laboratories, implantation rooms and operating theatres."
Prof. Dr Gerhard Hindricks
Overall Head of Rhythmology at the DHZC

Outpatient clinics
In our cardiology outpatient clinic, we offer comprehensive care for patients with all types of heart disease, including pacemaker and defibrillator checks.
Patients with cardiac arrhythmia can contact the specialist cardiological outpatient clinics in our hospital. We offer a consultation hour for patients with cardiac arrhythmia and atrial fibrillation as well as a pacemaker and defibrillator consultation hour.
For inpatients:
Patient management
T: +49 30 450 513 021
For outpatients:
Cardiological university outpatient clinic
T: +49 30 450 513 150
Hotline for medical colleagues:
Rhythm hotline
T: +49 30 450 513 110
For inpatients:
T: +49 30 450 565 400 (after the announcement: 1)
For outpatients:
T: +49 30 450 565 400 (after the announcement: 2)
Hotline for medical colleagues:
T: +49 30 450 665 445
For inpatients:
Patient management
T: +49 30 450 513 747
For outpatients:
Cardiological university outpatient clinic
T: +49 30 450 513 717
Hotline for medical colleagues:
Rhythm hotline
T: +49 30 450 513 636
Patient contact for inpatient stays / referral:
T: +49 30 4593 2250
einbestellung@dhzc-charite.de



