Cardiac arrhythmia
Cardiac arrhythmias have various causes. They are characterised by a rhythm that is too slow (bradycardia), too fast (tachycardia) and/or irregular. Many of these disorders are not immediately dangerous; the spectrum is wide. However, ventricular fibrillation is immediately life-threatening and must be treated immediately with life-saving measures.
Cardiac arrhythmias are widespread. Every year, around 400,000 people in Germany are hospitalised due to cardiac arrhythmias. Depending on the type and severity of the arrhythmia, various forms of therapy can be considered: conservative drug treatments, ablation treatments and the implantation of a defibrillator or pacemaker.
If the heart beats too fast or too slow
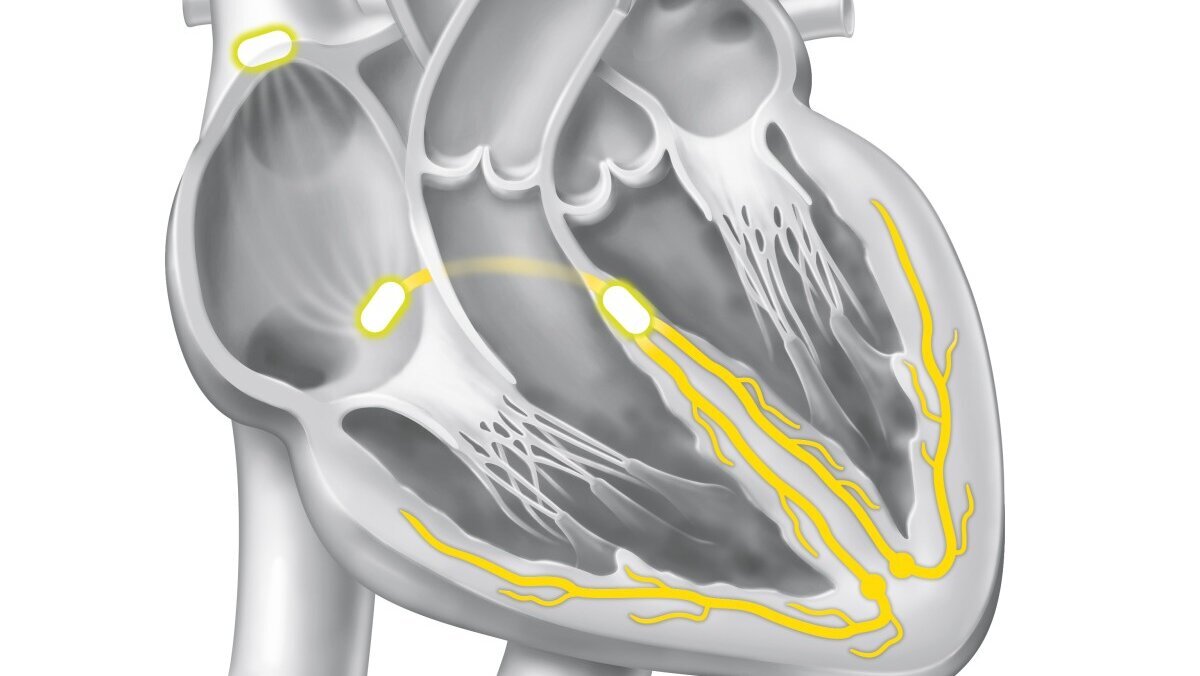
Graphical representation of a cardiac arrhythmia.
The normal heartbeat
At rest, the heart normally beats 60 to 70 times per minute. In order for it to pump blood through the body, an electric current flows through the heart and excites the heart muscle cells, which then contract.
The rhythm generator for the electrical impulses is the sinus node, which is located in the right atrium. It generates electrical impulses that are transmitted via the atria to the atrioventricular node (node between the atrial and ventricular levels) and from there to the ventricles. In this way, the individual heart compartments can work in a coordinated manner. If this rhythm is disrupted, a cardiac arrhythmia occurs.
Forms of cardiac arrhythmia
A slow heartbeat can have many causes. These include taking certain medications, disorders of the sinus node or disorders of the conduction between the atria and the ventricles (AV node disease). Signs of bradycardia include dizziness, nausea, shortness of breath or a general drop in performance. Some sufferers even fall unconscious.
If the heart beats too slowly, a cardiac pacemaker may need to be used.
Tachycardic arrhythmias can have different causes and occur at different locations in the heart, depending on the underlying heart disease. A distinction is made between tachycardias that occur in the atria of the ventricles (supraventricular tachycardias) and those that occur in the ventricles themselves (ventricular tachycardias). If left untreated, the latter can often lead to acute emergency situations, circulatory arrest and ultimately sudden cardiac death.
Fast cardiac arrhythmias from the atria are called supraventricular tachycardias. Those affected can suffer from palpitations, dizziness, breathlessness, chest pain, a feeling of inner restlessness and even loss of consciousness. However, this form of arrhythmia is only very rarely life-threatening.
These include:
AVNRT (AV nodal reentry tachycardia) and AVRT (AV reentry tachycardia, in the presence of an additional conduction pathway/WPW syndrome): These are the most common cardiac arrhythmias in young people with healthy hearts. The basis is an altered or even an additional electrical connection between the atrium and ventricle. In both forms, electrical impulses can not only travel from the atrium to the ventricle, but also back to the atrium again due to the special properties. This results in a circular excitation (reentry) with sometimes very high heart rates (200/min.)
Typical atrial flutter: The cause of this cardiac arrhythmia is an electrical reentry around the heart valve of the right atrium (tricuspid valve). Here the pulse is often increased, but regular. Heart rates of around 150/min usually occur. During exertion, the heart rate can rise above 250/min and thus become life-threatening.
Atrial fibrillation: The most common cardiac arrhythmia that occurs in the atria is atrial fibrillation: This causes circular excitations of different sizes in the atria. Only some of the chaotic electrical signals from the atria can reach the ventricles (this control function is performed by the AV node). The heart beats irregularly and, despite everything, often too fast. Atrial fibrillation is not immediately dangerous, but should be clarified by a doctor. This is because it can have serious consequences such as a stroke or heart failure.
Atrial tachycardia: This cardiac arrhythmia can occur in both healthy people and patients with heart disease (e.g. after heart surgery). It is caused either by electrical misfiring in the ventricle (ectopic atrial tachycardia), which fires its impulses into the heart, or by circular electrical excitation (reentry, usually atypical atrial flutter).
The cardiac arrhythmia can occur as an attack or be permanent.
Ventricular tachycardia is a cardiac arrhythmia in which the main chambers beat far too fast and no longer fill and empty with enough blood. Those affected feel very unwell, experience palpitations, dizziness, shortness of breath and chest tightness, can lose consciousness and, in the worst case, can lead to sudden cardiac death.
In ventricular fibrillation the ventricles are electrically stimulated so quickly and in an uncoordinated manner that cardiovascular arrest effectively occurs. Life-saving measures such as cardiac massage and the use of an external defibrillator must be started immediately.
Causes and risk factors
There are many causes of cardiac arrhythmia. They can occur unexpectedly and for no apparent reason at any age. However, the risk increases with age.
In many cases, the underlying cause is a cardiovascular disease, e.g. hypertension, a heart attack, a valvular heart disease or heart failure. Hormonal imbalances are also a possible cause.
Cardiac arrhythmias can also occur in young and healthy people. It can be triggered by the consumption of alcohol, caffeine, drugs or certain medications. These stimulate the central and autonomic nervous system, which stimulate the heart to beat faster.
Stress, nervousness or anxiety can also favour cardiac arrhythmias.
Symptome
Symptoms of a slow heartbeat (bradycardia)
A slow heartbeat is not always pathological. The condition only becomes dangerous when too little blood reaches the brain and organs. Those affected notice this, for example, through dizziness, shortness of breath, nausea and sweating. Other possible symptoms are tiredness, drowsiness and poor performance or visual disturbances. In some cases, those affected may faint. Slow cardiac arrhythmias associated with the above symptoms almost always require treatment.
Symptoms of a rapid heartbeat (tachycardia)
If the heart beats too fast at rest, those affected usually feel their heart pounding or racing. This is often accompanied by restlessness and nervousness, sometimes also by anxiety. Other possible symptoms are dizziness, shortness of breath or chest pain. Confusion, drowsiness or unconsciousness can only occur if the heart rate is very fast (> 200/min).
Attacks of palpitations that are not due to physical exertion or stress should be clarified.
Symptoms of cardiac arrhythmia
A heartbeat that is too fast can manifest itself in dizziness, shortness of breath or chest pain, among other things.
(Image: pixabay)

Diagnostic
Cardiac arrhythmias can be reliably detected by electrocardiogram (ECG) . This reflects the patient's electrical heart activity.
In some patients, cardiac arrhythmias only occur occasionally. In these cases, a long-term ECG measurement is necessary for a clear diagnosis. An ECG device, which the patient wears on a belt, records the electrocardiogram over a period of 24 to 72 hours. Electrodes are attached to the patient's skin for this purpose.
For rarer arrhythmias that cannot be recorded with long-term measurements, we at the DHZC offer recording with a so-called "loop recorder". With an external loop recorder, the device is worn on a belt and the ECG is recorded via electrodes attached to the skin. The measurement is triggered by the patient by pressing a button as soon as an arrhythmia is detected. The implantable "Loop Recorder", on the other hand, is inserted under the skin near the chest. It can record the heart rhythm for up to three years.
In addition to the ECG, we offer other diagnostic methods at the DHZC for the individual clarification of a cardiac arrhythmia. These include the creation of X-ray images or echocardiography, an ultrasound examination of the heart. You can find more information on our page on diagnostics.
Diagnosis with the ECG
Cardiac arrhythmias can be reliably diagnosed using an electrocardiogram.
(Image: DHZC)

To treat a rapid heartbeat, we offer various therapeutic approaches:
Defibrillators
Patients at risk: those with ventricular tachycardia must have a defibrillator implanted to protect them from sudden cardiac death. Sudden cardiac death is mainly caused by rapid (tachycardic) cardiac arrhythmias: Ventricular fibrillation causes the heart rate to become so fast and uncoordinated that the heart stops pumping blood to the body - leading to death within minutes.
The only way to stop this ventricular excitation at present is defibrillation. This involves delivering an electric shock through the heart either via two electrodes attached to the chest (external defibrillator) or via two electrodes located in the body (implantable cardioverter defibrillator ICD). This can interrupt the electrical activity in the heart chambers and restore the normal heart rhythm.
- Certain medications can be used to "slow down" the heart rate without explicitly treating the underlying arrhythmia. This so-called frequency-limiting therapy is suitable for many patients with atrial fibrillation, for example.
- Another option is rhythm-preserving therapy. This involves converting the heartbeat to normal sinus rhythm and keeping it stable with medication.
- Maintaining the sinus rhythm can also be achieved through ablation treatment (catheter ablation). This involves inserting special probes into the heart via a cardiac catheter, which can be used to sclerotise specific areas of heart muscle tissue that are causing the arrhythmia. As a rule, normal heart function is not affected. In many cases, better results can be achieved with ablation treatment than with drug therapy. In some diseases, such as atrial flutter, a cure is possible with a single ablation treatment.
- Transvenous and subcutaneous systems are available for implantation. We perform both forms of implantation at the DHZC.
- In transvenous systems an electrode (probe) is inserted into the right heart via a vein in the arm. This is connected to the actual ICD, which is inserted under the skin or under the muscle itself at the level of the chest muscle. The defibrillator consists of a battery, the capacitors and the electronics. It monitors the patient's own heartbeat and triggers an electric shock if necessary.
- In subcutaneous systems the electrode is not inserted into the heart via a vein, but implanted under the skin. The advantage of this is that the probe can be removed easily and safely in the event of a fault. In most cases, a normal life adapted to the heart disease is possible after ICD implantation.
Although not all bradycardias need to be treated, some patients whose heart beats too slowly need a cardiac pacemaker. This stimulates the heart to beat faster and thus also eliminates the symptoms that occur with slow cardiac arrhythmias, such as dizziness.
Cardiac pacemakers
Not every bradycardia needs to be treated with a pacemaker. The use of a pacemaker is particularly recommended if symptoms or physical complaints occur below the slow heart rate of usually less than 40 beats per minute or pauses of more than five seconds. The doctors at the DHZC have many years of experience in the implantation of pacemaker and defibrillator systems.
When a pacemaker is implanted, electrodes (probes) are inserted into the right heart (atrium and/or ventricle) via a vein in the arm, for example in the area of the collarbone. They recognise the patient's own heartbeat and stimulate the heart if it is beating too slowly. In this way, a diseased sinus or AV node can be replaced. The electrodes are connected to the actual pacemaker, which is inserted under the skin or under the muscle itself at the level of the chest muscle. This consists of a battery and the electronics.
To ensure that the pacemaker is working properly, it must be checked every six to twelve months. With modern devices, this check can be carried out at home, saving older patients in particular a trip to the doctor's surgery. The pacemakers can also be reprogrammed and thus adapted to the patient's individual needs.
In most cases, a completely normal life is possible after pacemaker implantation.
At the DHZC, we use the latest generation of pacemakers: cable- and probe-free, capsule-like devices that are inserted via a catheter and the vein.
They can be inserted gently and removed again if necessary. They have an unprecedented battery life and enable wireless dual-chamber pacing for the first time.

Outpatient clinics
In our cardiological outpatient clinics, we offer comprehensive care for patients with all types of heart disease, including pacemaker and defibrillator checks.
Patients with cardiac arrhythmia can contact the specialist cardiological outpatient clinics at the various DHZC locations. We offer a consultation hour for patients with cardiac arrhythmia and atrial fibrillation as well as a pacemaker and defibrillator consultation hour.
You can find all contact details and availability here:
Appointment allocation:
Secretariat
T: +49 30 450 513 072
kardio-ccm-ambulanz@dhzc-charite.de
Location:
3rd level of the bed tower (Luisenstr. 64, registration 3A)
Accessibility:
Monday to Friday from 8:00 - 13:30
Patients with statutory health insurance
T: +49 30 450 513 717
F: +49 30 450 513 996
kardio-cbf-hsa@charite.de
Patients with private insurance
T: +49 30 450 513 870 /-871
F: +49 30 450 7 513 901
privat-kardio-cbf@charite.de
In our cardiology outpatient clinic, we offer comprehensive care for patients with all types of heart disease, including pacemaker and defibrillator checks. We also have an emergency outpatient clinic for acute chest pain (Chest Pain Unit). We also look after inpatients from the German Heart Centre at Charité.
Accessibility and contact:
Monday to Friday from 7:30 - 16:00 (by appointment)
T: +49 30 450 565 400
F: +49 30 4593 2419
For referring physicians: Rhythmology at the DHZC
At the German Heart Centre of the Charité (DHZC) in Berlin, a large team of specialists work in the field of rhythmology under the direction of Prof. Dr Gerhard Hindricks. We treat outpatients and inpatients with cardiac arrhythmias at four DHZC clinics.



