Heart and lung transplantation at the DHZC
Heart, lung and combined heart-lung transplants have been performed at the Deutsches Herzzentrum der Charité (DHZC) for more than 30 years. This has resulted in one of the largest and most successful transplant programmes in Germany. As a supra-regional centre, we care for patients with severe heart or lung diseases from all over Germany. For these patients, a transplant is often the last hope. Our transplant outpatient clinic is of central importance here: more than 600 patients are cared for in our transplant follow-up programme.
An experienced and interdisciplinary team at the DHZC specialises in the diagnosis and treatment of terminal heart and lung diseases that require a transplant. Cardiologists, pneumologists and cardiothoracic and vascular surgeons work hand in hand with nursing staff, nutritionists and psychologists to ensure that patients receive individualised care.
The heart and lung transplant programme at the DHZC
In 2023, 38 hearts and 10 lungs were transplanted at the DHZC. A total of 330 heart and heart-lung transplants were performed throughout Germany in 2020 (source: German Organ Transplantation Foundation DSO).
A transplant is the best possible treatment alternative for serious diseases of the heart or lungs. On the one hand, this increases the patient's chances of a high quality of life in the long term, but on the other hand, it is a complicated operation that can lead to considerable physical and emotional stress.
As the heart and lungs are closely connected via the blood circulation, diseases of one organ can also cause impairment of the other. If both organs are damaged, a heart-lung transplant is performed if possible.
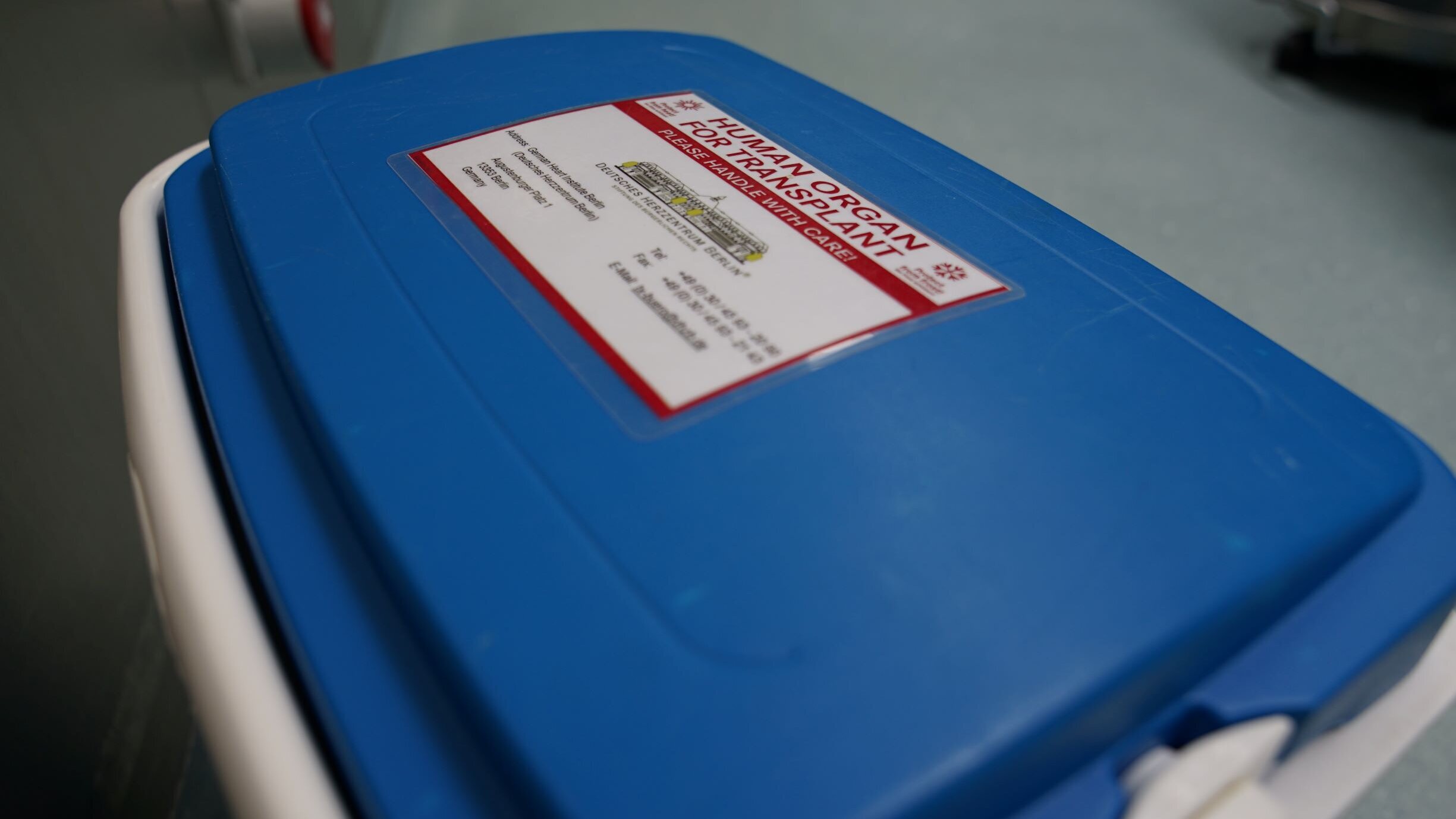
Before the organ is harvested, the medical data of the donor organ is carefully checked. After removal, the organ is transported in a special box. It is cooled and preserved with a special solution to prevent tissue damage.
(Image: DHZC).
How is organ donation organised?
In a heart and/or lung transplant, an incurably ill organ is replaced by that of a brain-dead donor. Brain death is determined independently by two specially trained doctors.
In Germany, organ donation is regulated by the Transplantation Act. This law strictly separates the areas of organ donation, organ procurement and organ transfer in order to rule out conflicts of interest. The German Organ Transplantation Foundation (DSO) coordinates and supports the processes of determining the donor's brain death and organ removal.
The Eurotransplant Foundation in the Netherlands is responsible for the procurement of all donor organs that are removed in eight European countries, including Germany. Transplant centres carry out the organ transplantation.
The German Heart Centre Berlin is one of the 25 centres for heart transplantation and 16 centres for lung transplantation in Germany.
Who gets a donor organ?
An organ transplant is only possible if there is no other promising therapy to treat the disease. As there are too few suitable donor organs, strict criteria apply when allocating organs. The decisive factors are primarily those that make a transplant urgently necessary and increase the chances of success of the procedure.
Whether a patient is eligible for a transplant is decided by the treating physicians according to globally recognised guidelines. For example, patients suffering from malignant tumours or other serious illnesses are excluded from a transplant.
If a patient is eligible for a transplant, they can be actively listed with Eurotransplant . Eurotransplant allocates organs according to the following criteria:
- Matching blood group
- donor and recipient are as similar in size and weight as possible (+/- 15 per cent)
- Furthermore, the urgency is taken into account according to the severity of the clinical picture.
The waiting time can vary significantly from patient to patient and can take up to several years.
Patients with acutely life-threatening and incurable heart failure for whom a donor organ is not available in time are therefore often given an artificial circulatory pump. These systems are called VADs (ventricular assist devices) or artificial heart systems and consist of a small pump that the doctor inserts directly into the patient's heart.
Thanks to improved techniques and surgical procedures, artificial heart systems are increasingly becoming a longer-term alternative to transplantation.
The ischaemia time, during which the removed donor organ is not supplied with blood, must be kept as short as possible in order to avoid damaging the organ. It must not exceed four hours.
(Image: DHZC/Maier)

The process of an organ transplant
Once brain death and the deceased's willingness to donate have been determined by the DSO at the donor centre, Eurotransplant is informed about the available organ.
The foundation, which is based in the Netherlands, then determines which recipient is most suitable and notifies the transplant centre where the patient is being treated.
There, a surgeon checks the medical data provided by the donor organ. If he or she decides to accept it, a specialised team of doctors will make their way to the donor hospital.
Once the team has arrived at the donor centre, it takes over the removal of the organ. This is the start of the ischaemia period, during which the organ is not supplied with blood. This must be kept as short as possible to prevent damage to the organ.
At the same time as the organ is removed, the recipient is prepared for the transplant in the operating theatre. When the removal team sets off on its return journey, the operation begins. This ensures that the ischaemia time can be kept as short as possible. In the case of donor hearts, for example, the ischaemia time should not exceed four hours.
Organ donation after cardiac death (DCD)
In Germany, organs may currently only be donated after brain death. This refers to the complete, irreversible loss of all brain functions – the cerebrum, cerebellum, and brain stem are irretrievably destroyed. Although the patient is still on a ventilator, they are medically and legally dead.
In many other European countries, organ donation after cardiac death is also permitted. This is referred to as donation after circulatory death (DCD). Organ donation becomes possible when the heart stops beating irretrievably and there is no longer any blood circulation.
Forms of DCD
• In controlled DCD (cDCD), circulatory arrest occurs when life-sustaining measures are discontinued in patients with a hopeless prognosis. After cardiac arrest, a specified waiting period is observed before organ donation may begin. The advantage is that the process can be planned and the transplant team can be prepared.
• In uncontrolled DCD (uDCD), circulatory arrest occurs unexpectedly, for example after unsuccessful resuscitation in the emergency room or outside the hospital. Once it is clear that the patient cannot be revived, organs can be removed according to established protocols. The advantage is that the number of donations can be significantly increased, even though the procedures must be carried out very quickly.
Differences from brain death
• In the case of organ donation after brain death, the patient is still on artificial ventilation. The organs remain well supplied with blood and the procedures can be planned.
• In the case of DCD donation, the organs must be secured very quickly after cardiac arrest because they can be damaged without blood flow.
Experience in Europe
• In Spain, both controlled and uncontrolled DCD are performed. Around one-third of all donors now come from this group.
• France has established uncontrolled DCD, especially in large cities.
• Controlled DCD has also been introduced in the Netherlands, Belgium, the United Kingdom, and Switzerland. This has led to a significant increase in the number of donors.
Conclusion
Organ donation after cardiac death (DCD) is an additional procedure that is successfully used in many countries to help more patients on waiting lists. In Germany, this procedure is not yet legally permitted, but the discussion about it is becoming increasingly intense.
Further information on organ donation in Germany and Europe, including numerous figures and diagrams, can be found here:
Progress in heart transplantation
At the DHZC, we are the first clinic in Germany to use a new system for preserving donor hearts, which enables better organ function and longer transport times. During transport, the organ is supplied with a special nutrient and preservative fluid via a pump. The new technology should enable even better function of the donor organs and significantly longer transport times. Following very good results in animal experiments, it is now being used in human hearts as part of an authorisation study. Confirmation of the efficiency of this system would have significant consequences for transplantation medicine.
The system consists of a device called the ‘XVIVO Heart Box’ for transport and a special solution for preserving the organ. Before transport, the device is filled with a newly developed nutrient and preservation solution. After removal, the donor heart is first connected to the circulation pump in the ‘Heart Box’ and then stored floating in the nutrient and preservation solution. During transport, the organ is continuously supplied with fresh oxygen.
The XVIVO ‘Heart Box
The ‘Heart Box’ from XVIVO is designed to enable longer transports of donor organs.
It essentially contains a cooling system, a circulatory pump and an oxygenator, in other words an artificial lung.
(Image: DHZC)

After the transplant
Immediately after the operation, patients are transferred to the intensive care unit while still under anaesthetic. There they are monitored around the clock by doctors and nurses. During the operation and in the initial period afterwards, patients are artificially ventilated with a ventilator. As soon as they are able to breathe sufficiently on their own, the breathing tube is removed and the patients can eat independently again.
Immediately after the operation, physiotherapy care begins in the intensive care unit. Specialised breathing trainers and physiotherapists perform breathing and muscle training exercises with the patients.
As soon as their physical condition allows, patients are transferred to our transplant ward WD3. They spend the time until rehabilitation on the heart failure and transplant ward, which is certified by the German Society of Cardiology. Under careful medical and nursing supervision, patients are prepared here for their discharge from the hospital.
In order to check organ function, the team of doctors at the DHZC performs numerous examinations on patients in the first few weeks after the transplant. These include blood samples, X-rays, ECG and echocardiography after a heart transplant, as well as lung function tests and bronchoscopy after a lung transplant. Before patients are discharged into rehabilitation, we carry out a cardiac catheterisation with a heart muscle biopsy and, if necessary, a cardiac MRI for heart transplant patients in order to rule out rejection of the donor organ.
Transplant ward WD3
Heart and lung transplant patients spend the first post-operative phase on the WD3 ward. The WD3 team also cares for long-term transplant patients who have to be hospitalised as part of routine examinations, infection therapies or rejection treatments.
(Image: DHZC)
Prof Felix Schönrath is Senior physician for the Transplantation Department at the DHZC (Image: DHZC).


Our transplant outpatient clinic
After discharge from the clinic and the rehabilitation centre, the transplant outpatient clinic at the DHZC is the permanent point of contact for transplant patients, alongside their family doctor and specialist. Specialised doctors are available to answer all questions relating to transplantation. The state of health and function of the new organs are closely monitored at regular examination appointments. The examinations carried out include ECG and echocardiography appointments as well as X-rays and lung function tests.
The blood levels of immunosuppressants are also regularly determined and analysed. This is because the new organ would normally be recognised by the body's defence system as foreign tissue and attacked - comparable to the incompatibility between different blood groups. For this reason, the patient must takelifelong medication after the transplant to regulate the defence system, so-called immunosuppressants. This is the only way the organ can be accepted by the body and function properly.
After the transplant, patients initially have to visit the outpatient clinic very often. Over time, however, the likelihood of a rejection reaction decreases so that check-ups become less frequent. The transplant outpatient clinic also provides advice on acute questions and problems and also looks after patients before the operation while they are waiting for a donor organ. Doctors and nurses work closely together.
Heike Bettmann, Head of Nursing at the transplant outpatient clinic (Image: DHZC).
- Mehr über die Transplantationsambulanz

Guide for patients
We have summarised everything patients need to know about the time after an organ transplant in an easy-to-understand guide:
Guide for patients after transplantation
transplantiert e.V. - Patients help patients
The association transplantiert e.V. has been supporting people and their relatives who are waiting for a donor organ or living with a donor organ for many years. The volunteers live with transplanted organs themselves and are therefore able to provide experienced assistance and support in a special way. On the transplantiert e.V. website, you will find a wealth of information on the subject of organ transplantation and can contact the organisation.
Currently, transplantiert e.V. offers a website with information on transplant patients and the coronavirus. The most important questions about the risks and protection of transplant recipients are answered at https://tx-corona-info.de/. Interested parties can also find videos, current articles in a blog and infographics on the topic.
The Verein transplantiert e.V. has been supporting people and their relatives who are waiting for a donor organ or living with a donor organ for many years.


