Heart attack
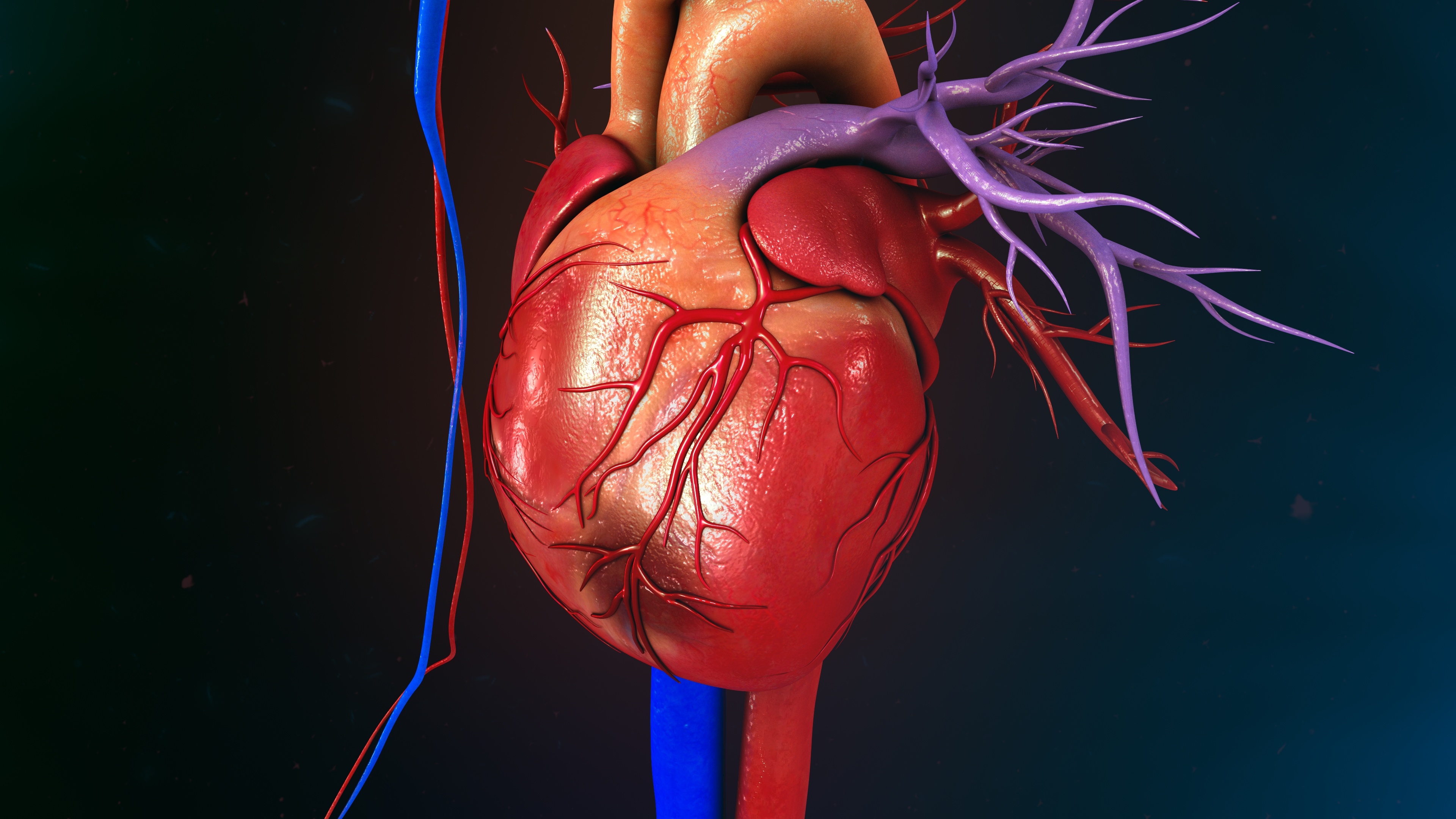
A heart attack (medically: myocardial infarction) is caused by the blockage of a coronary artery. If the blocked coronary artery is not opened by a cardiac catheterisation with PCI (percutaneous coronary intervention = ‘balloon dilatation and stenting’), the heart muscle dies at this point. To minimise the death of heart muscle tissue, the vessel must be reopened as quickly as possible. Those affected must therefore be taken to hospital as quickly as possible, where cardiac catheterisation can be carried out around the clock.
Despite good medical care, 35 per cent of patients still die in the first year after a heart attack. This is why we now speak of chronic coronary syndrome: heart attack patients must be monitored and treated for the rest of their lives. The earlier the heart attack is recognised and treated, the better the prognosis.
Cause
The occlusion of a coronary artery is caused by the rupture of an atherosclerotic plaque, i.e. at a point in the artery wall that is diseased due to risk factors such as high blood lipids, diabetes, smoking or high blood pressure. When the plaque ruptures, blood platelets accumulate and block the vessel. A thrombus is formed, which stops the blood flow.
Important to know:This disease affects all arteries in the body.
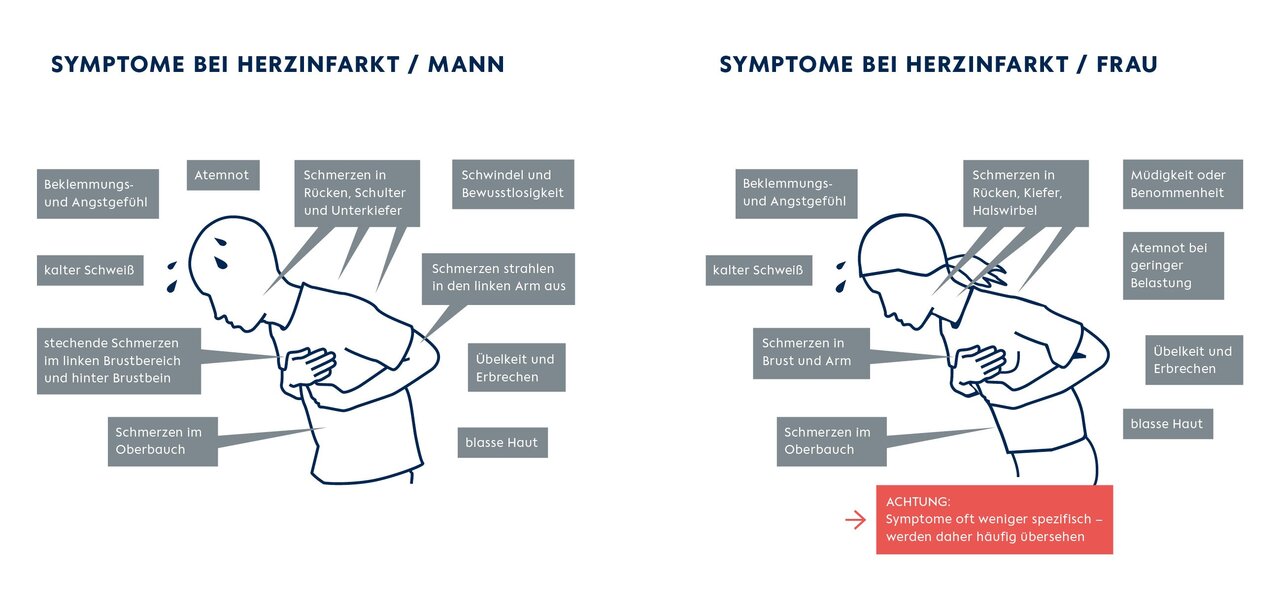
Symptoms of a heart attack
- The patient has severe pain (burning, pressure, tightness) behind the breastbone. This pain often radiates to the left arm, shoulder, lower jaw or upper abdomen.
- The patient may be very restless and feel great anxiety (fear of death).
- In the worst case, cardiovascular arrest may occur.
- Other rather unspecific symptoms are nausea, vomiting or shortness of breath.
Women often have a different set of symptoms: while the majority of affected men experience classic chest pain, only around a third of women do. Non-specific symptoms, on the other hand, are more common in women. These include shortness of breath, nausea and vomiting as well as discomfort in the upper abdomen.
Such symptoms are often not immediately recognised as heart attack symptoms - they are therefore often taken less seriously. This is why women with a heart attack are hospitalised later on average than men affected by a heart attack
A heart attack can happen ‘out of the blue’. However, the majority of those affected have often had symptoms of coronary heart disease (CHD), such as angina pectoris or shortness of breath, for some time. It is therefore important to recognise these symptoms and initiate treatment at an early stage.
If chest pain and/or shortness of breath occur even with the slightest exertion or even at rest, call an emergency doctor immediately!
Diagnosis and therapy
If symptoms are present, the diagnosis of myocardial infarction is made using an electrocardiogram (ECG) and laboratory values.
The ECG is used to differentiate between ST-segment elevation myocardial infarction (STEMI; typically with complete occlusion of a coronary vessel) and non-ST-segment elevation myocardial infarction (NSTEMI). Important to know: both are dangerous!
Once a heart attack has been diagnosed, doctors widen the blocked vessels as quickly as possible using acardiac catheterand insert a stent to keep the vessel permanently open.
The effects of the heart attack depend on where the vessel becomes blocked and how quickly the vessel is reopened.
If a heart attack has been diagnosed, the doctors widen the blocked vessels with a cardiac catheter and insert a stent to keep the vessel permanently open (image: DHZC).

Consequences of a heart attack
Despite good medical care, the mortality rate for myocardial infarction is still high: more than a third of all patients die in the first year after a heart attack, and the mortality rate for STEMI patients in Europe is still up to 10 per cent in the following year. This is why it is now referred to as chronic coronary syndrome, which requires lifelong monitoring and treatment.
Even if patients survive the myocardial infarction, serious complications and secondary diseases can occur that affect their lives in the long term. These include, in particular, heart failure and heart valve defects, such as leaks in the heart valves as a result of heart failure.
Mortality and complications can usually be significantly reduced or even prevented if the disease is recognised early and treated quickly.
The earlier a heart attack is recognised and treated, the greater the patient's chances of survival and the lower the risk of complications and secondary diseases later on.
The Chest Pain Unit at the DHZC
Please note: if you experience acute chest pain, you should always call an emergency doctor by dialling 112!
The DHZC has a Chest Pain Unit (CPU) certified by the German Society of Cardiology, i.e. a diagnostic and therapy unit for the rapid treatment of patients with acute chest pain. Standardised diagnostic procedures are used to check without delay whether a heart condition is the cause of the chest pain. Taking into account the latest national and international guidelines, experienced teams use standardised procedures to diagnose and treat the patient in the shortest possible time. The individual severity of the illness, the needs and the individual risk of the patient are of course taken into account.
Chest Pain Unit (CPU)
The Chest Pain Unit is an interface between the cardiological outpatient clinic, cardiological monitoring ward, intensive care unit and cardiac catheterisation laboratory. It is under the medical direction of Prof Dr Philipp Stawowy.
The CPU has been repeatedly certified by the German Society of Cardiology.
Berlin-Brandenburg Heart Attack Register e.V.
The cardiology clinics of the DHZC at the Wedding, Mitte and Steglitz sites actively participate in the Berlin-Brandenburg Heart Attack Register (B2HIR).
The B2HIR serves to ensure the quality of care for patients with heart attacks in the participating clinics. It uses the data collected in the clinics to analyse whether the clinics are treating their patients in accordance with the guidelines.