Pacemakers & defibrillators
Pacemakers (HSM) are devices that are used to treat patients with a slow heartbeat (bradycardia).
Some patients with cardiac arrhythmia or pronounced cardiac insufficiency who are at increased risk of sudden cardiac death must be implanted with defibrillators. These medical devices deliver electric shocks via electrodes to normalise the disturbed heart rhythm.
Pacemaker
Bradycardia is usually caused by a disorder of the sinus node (the rhythm generator beats too slowly) or the AV node (the electrical impulse is not transmitted correctly). The symptoms can occur either constantly, only occasionally or exclusively during exercise. The indication for a pacemaker arises from the treatment of symptoms (e.g. dizziness, loss of consciousness or limited exercise capacity) or for prognostic reasons in order to be able to control the further course of the disease (e.g. prevention of syncope, cardiac arrest).
Not every bradycardia needs to be treated with a pacemaker.
Implantation and mode of operation
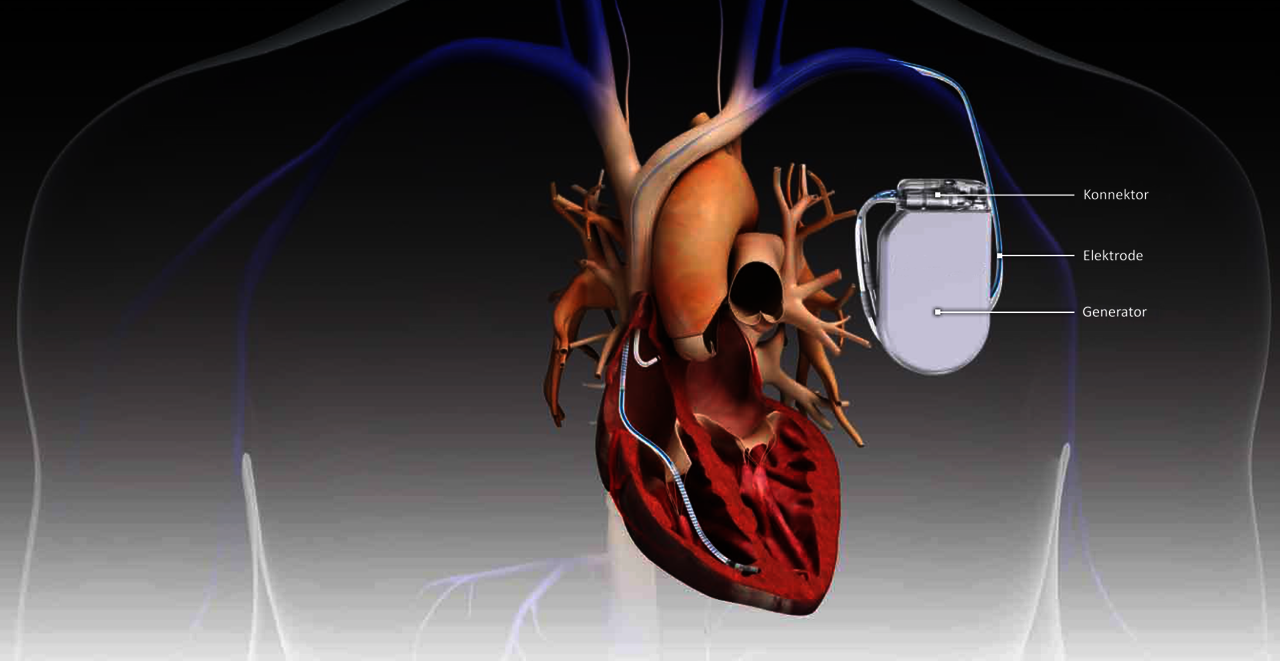
When a pacemaker is implanted, electrodes or probes are inserted into the right heart (atrium and/or ventricle) via a vein in the arm, for example in the area of the collarbone. The purpose of the probes is to recognise the patient's own heartbeat. Today's pacemakers do not intervene if the patient's own heart beats fast enough.
If the heart is too slow, it is stimulated electrically via the electrodes. In this way, a diseased sinus or AV node can be replaced. The electrodes are connected to the actual pacemaker, which is then inserted under the skin or under the muscle itself at the level of the chest muscle. This consists of a battery and the electronics. If the battery charge slowly becomes too low, the entire pacemaker (except for the electrodes) must be replaced.
To ensure that the HSM and the electrodes function properly, they must be checked every six to twelve months. This is done using a special device that is placed over the pacemaker and makes contact with it. In addition to monitoring, the pacemaker can also be reprogrammed to meet individual needs.
Modern pacemakers can also be checked from home, so that older patients in particular are spared the trip to the doctor's surgery. However, they should still be seen in person once a year.
In most cases, a completely normal life is possible after the pacemaker implantation. Most electrical devices pose no danger to the HSM.
State-of-the-art pacemakers
At the DHZC, we use the latest generation of pacemakers: cable-free and probe-free, capsule-like devices that are inserted via a catheter and the vein.
These new devices can be inserted gently and, if necessary, removed again. They have an unprecedented battery life and also enable wireless dual-chamber stimulation for the first time.

Defibrillators
The implantation of an ICD (implantable cardioverter defibrillator) is the most sensible and safest method of preventing sudden cardiac death in patients at risk.
Sudden cardiac death is mainly caused by rapid (tachycardic) cardiac arrhythmias . This causes a circular (ventricular tachycardia) or disorganised electrical activity (ventricular fibrillation) in one of the two chambers of the heart. The heart rate becomes so fast that the heart can no longer pump blood into the body. This leads to death within minutes. Defibrillation is currently the only way to stop this abnormally fast ventricular excitation. This involves delivering an electric shock through the heart either via two electrodes attached to the patient's chest or via two electrodes (ICD) located in the body. This can interrupt the disorganised electrical activity in the ventricles and restore a normal heartbeat.
Who needs an ICD?
There are two indications for the implantation of an ICD: Firstly, patients who have already experienced such a cardiac arrhythmia (survived sudden cardiac death) and for whom there is no treatable reason for this event. Secondly, patients who are at an increased risk of sudden cardiac death. In particular, these are patients with pronounced cardiac insufficiency, certain heart muscle diseases or other changes that favour the occurrence of dangerous cardiac arrhythmias.
There are currently two systems that can be implanted: The established transvenous systems and the newer subcutaneous systems.
Similar to the implantation of a pacemaker, an electrode/probe is inserted into the right heart (atrium and/or ventricle) via a vein in the arm, for example in the area of the collarbone. This is connected to the actual ICD, which is then inserted under the skin or under the muscle itself at the level of the chest muscle. It consists of a battery, the capacitors and the electronics.
The difference to a pure pacemaker probe is the ability to deliver a current surge from the end of the electrode to the ICD unit. To ensure a current flow through the heart, the ICD is also predominantly used on the left side. The ICD monitors the patient's own heartbeat and therefore the heart rate.
If this exceeds a certain value (e.g. 180 beats per minute), it starts a programme to check the frequency and the probability of whether there really is a dangerous cardiac arrhythmia. If this is the case, an attempt is first made to normalise the heart rhythm in a ‘gentle’ manner. This is done by rapidly stimulating the heart (overstimulation). If this is not successful, the electric shock is triggered.
In contrast to transvenous systems, the electrode is not inserted into the heart via a vein, but implanted exclusively under the skin. The advantage of this is that if the probe malfunctions, explantation (removal of the probe) is much easier and less risky. With transvenous systems, such a malfunction occurs in 20 per cent of cases within ten years. One disadvantage is the lack of pacemaker function offered by the transvenous system.
If the battery charge slowly becomes too low, the ICD unit (except for the electrodes) must be replaced. To ensure that the ICD and electrodes function properly, they must be checked regularly (two to three times a year). This is done using a special device that is placed over the ICD and makes contact with it. In addition to monitoring, the ICD can also be reprogrammed to meet individual needs. Modern ICDs can also be interrogated from home, saving older patients in particular a trip to the doctor's surgery. However, they should still be seen in person once a year.
One of the risks of ICD therapy is so-called inadequate shock. This means that a shock is triggered even though there was no dangerous cardiac arrhythmia. This may be due to a rapid heart rhythm, for example, which is not dangerous, or because an electrode is defective.
In most cases, a normal life adapted to the heart disease is possible after ICD implantation.
Extraktion von Schrittmacher- und Defibrillatorsonden
Da immer mehr Schrittmacher und Defibrillatoren implantiert werden, wird es auch immer häufiger notwendig, diese Systeme wieder vollständig zu entfernen oder einzelne Sonden zu extrahieren. Gründe hierfür können unter anderem eine Infektion des Systems, die Fehlfunktion einer Sonde oder der durch eine Sonde bedingte Verschluss eines großen Blutgefässes sein.
Die Entfernung des Schrittmacher- bzw. Defibrillator-Aggregats selbst ist in der Regel unproblematisch, da es im Unterhautfettgewebe oder unter dem Brustmuskel platziert und gut zugänglich sind. Die schlauch- bzw. drahtförmigen Sonden eines solchen Systems, die über das Venensystem in die Herzkammern gelegt werden, können jedoch mit den Gefäßwänden oder dem Herzmuskel selbst verwachsen. Die Entfernung der Sonden ist je nach Ausprägung der Verwachsungen entsprechend komplex.
Probe extraction at the DHZC
A high level of medical expertise and excellent equipment are required to perform probe extractions successfully and safely. At the Deutsches Herzzentrum der Charité, these procedures are only performed by a small number of specially trained and highly experienced surgeons. These experts have a wide range of state-of-the-art specialised instruments at their disposal.
The minimally invasive probe extractions are performed in a so-called hybrid operating theatre with state-of-the-art imaging technology (X-ray and ultrasound systems).
In the extremely rare event of a serious complication, open cardiac surgery can be performed at any time without any further delay, if necessary with the aid of a heart-lung machine.