The Aorta
Diseases and their prevention, diagnosis and treatment
The aorta, also known as the main artery, is the largest artery in the human body. It transports oxygen-rich blood from the heart to the entire body through branching vessels. Almost five litres of blood flow through the aorta of an adult every minute. The blood in the body is transported by the pressure generated by the heart (blood pressure).
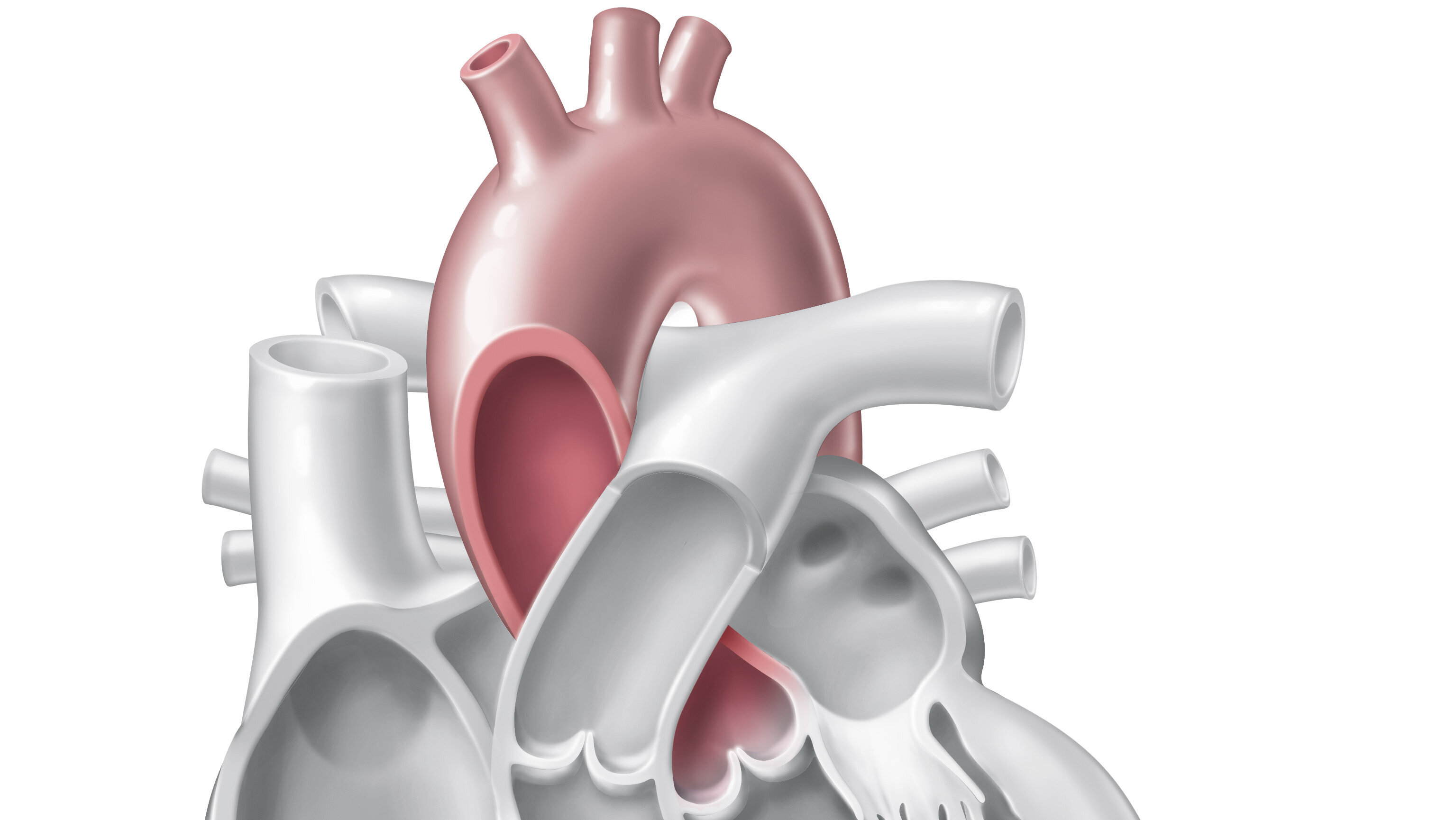
Schematic location of the aorta above the heart.
Anatomy
In an adult human, the aorta has a diameter of about 2.5–3.5 cm and a length of 30–40 cm. It resembles a walking stick in shape, with an arched beginning and a straight course down to the pelvic area.
The aorta originates directly at the left ventricle. This area is called the aortic root. The valve between the ventricle and the aorta is the aortic valve. The coronary arteries, which supply the heart muscle itself with oxygen-rich blood, branch off from the aorta directly at the heart.
From the heart, the aorta runs vertically upwards for about five to six centimetres. This section is called the ascending aorta. After that, the aorta curves to the left in the direction of the spine. The arteries that supply the head (the carotids), neck and arms originate from this section – the aortic arch.
The aorta then runs downwards parallel to the spine until it splits into the two large iliac arteries, the iliac vessels, at the level of the fourth lumbar vertebra. This descending part of the aorta is about 30 centimetres long in adults and is called the ‘aorta descendes’.
The upper section of the aorta – from the aortic root to where it passes through the diaphragm – is called the thoracic aorta. The section of the descending aorta below that is called the abdominal aorta. All the vessels that supply the abdominal organs branch off here, including those to the gastrointestinal tract, liver, kidneys and spleen. The aorta then divides into the iliac vessels, which supply the legs with oxygen-rich blood.
Aortic wall layers
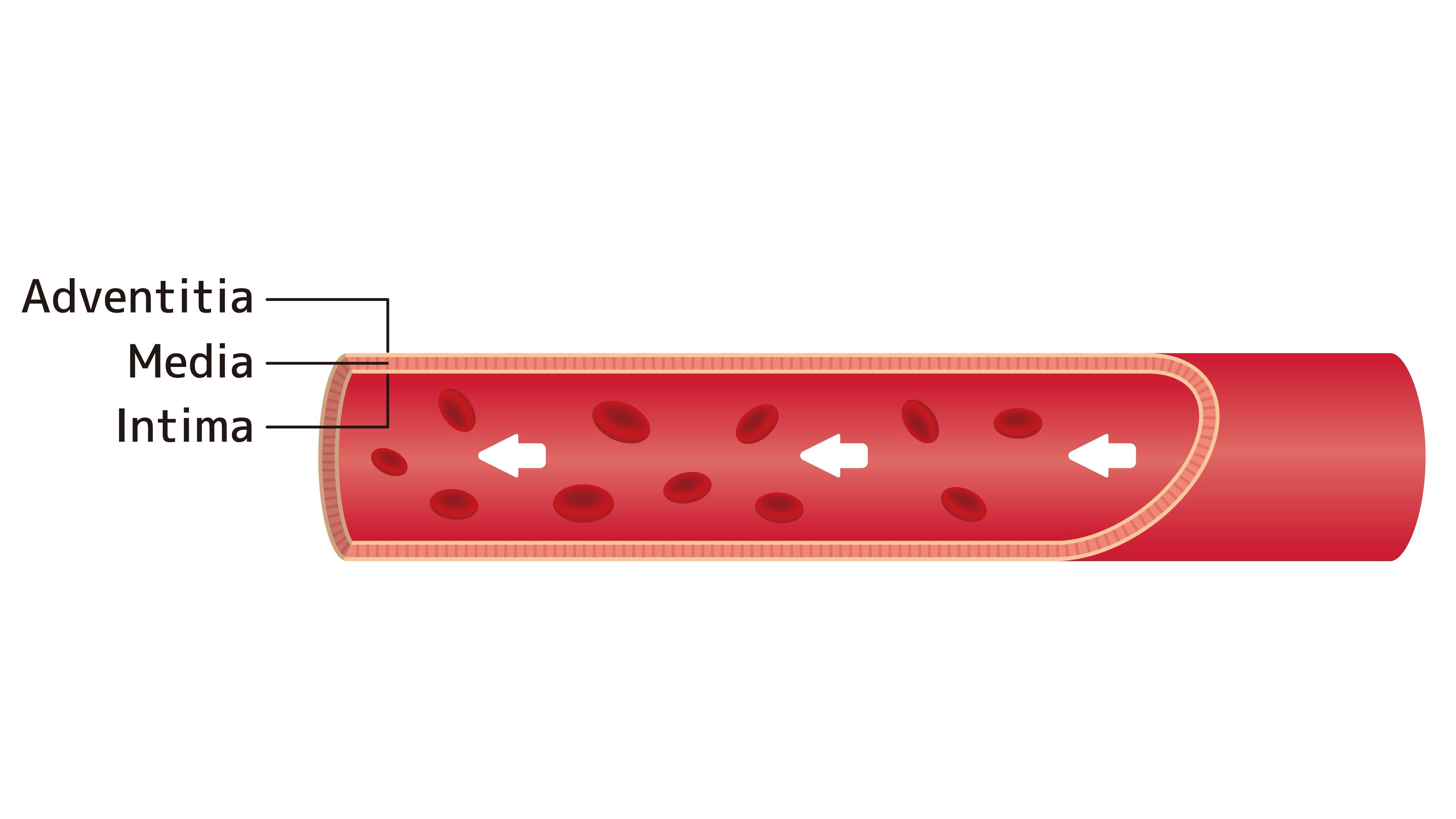
The wall of blood vessels basically consists of three layers called intima, media and adventitia. Each layer fulfils a different function.
The innermost layer forms the boundary with the interior of the vessels, the so-called lumen. It consists of a single layer of cells, the endothelium. The endothelium controls the passage of blood components into the surrounding tissue and is necessary for the exchange of gases and nutrients. Damage to the endothelium promotes the formation of blood clots (thrombi), for example to stop bleeding in the event of injury.
The middle and widest layer consists mainly of circular smooth muscle cells. The diameter of the individual vessels can be changed by tensing and relaxing these muscle cells, so that organs can be supplied with blood as needed. This layer also contains a large number of elastic and collagen fibres.
The adventitia, the outermost layer of the vessel wall, consists of connective tissue and embeds the aorta in the surrounding tissue. In addition, the adventitia contains tiny blood vessels, nerves and lymph vessels that supply the vessel itself.
The layers of the aorta
(Image: Adobe Stock).
Acute aortic diseases
Acute type A aortic dissection is one of the most urgent emergencies in cardiac surgery. Highly specialised experts with years of experience are available at the Deutsches Herzzentrum der Charité for every type of cardiac or vascular surgery, for intensive care, and for outpatient pre- and post-operative care.
Doctors will find a list of emergency numbers here.
Acute aortic diseases, including acute aortic syndrome, comprise various sudden conditions. These are often associated with severe pain and usually constitute an emergency. Acute aortic syndrome is divided into five classes, which we describe in detail on our aortic dissection page.
- Penetrating aortic ulcer (PAU)
- Intramural haematoma (IMH)
- Traumatic or iatrogenic aortic rupture
- Acute inflammation of the aorta
Chronic aortic disease
In Germany, cardiovascular diseases caused by arteriosclerosis are the most common causes of death. Put simply, the term arteriosclerosis refers to the pathological narrowing of an artery. This vascular narrowing occurs because blood lipids, blood clots, connective tissue and calcium are deposited in the vessel walls. Aortic diseases such as aortic aneurysm or aortic dissection are also greatly increased by arteriosclerosis.
In the case of an aortic aneurysm, all three layers of the vessel wall widen and the diameter of the vessel increases. You can find more information about this condition on our extensive page about aortic aneurysms.
Like aortic aneurysm, chronic aortic dissection is a slowly progressive disease of the aorta. It is very important to have regular check-ups to monitor the progression of the disease and to consult a doctor immediately if any new acute symptoms occur.
Risk factors
Personal factors and lifestyle habits, anatomical or genetic peculiarities and other concomitant illnesses can increase the risk of developing an aortic disease.
General risk factors
People between the ages of 60 and 90 are most often affected. Men are twice as likely as women to suffer from aortic dissection. Long-term uncontrolled high blood pressure (hypertension) increases the likelihood of an aortic aneurysm or aortic dissection occurring. This also applies to factors that change the structure of the blood vessels in the long term and promote the development of atherosclerosis. Atherosclerosis hardens the arterial walls, making them less flexible and more brittle. Factors that can contribute to this include lipometabolic disorders, diabetes mellitus and smoking.
Special life situations
Under certain conditions, aortic dissection can occur during pregnancy. The risk is higher if there is an underlying condition. In isolated cases, healthy women can also be affected. Demanding strength training, especially high-intensity weightlifting, can contribute to the development of aortic dissection due to a rapid increase in blood pressure during exertion. Cocaine use is also associated with an increased risk of aortic dissection.
Reconstruction of a bicuspid aortic valve
© www.IDHK.de 2012 (Illustration Jan Bazing)
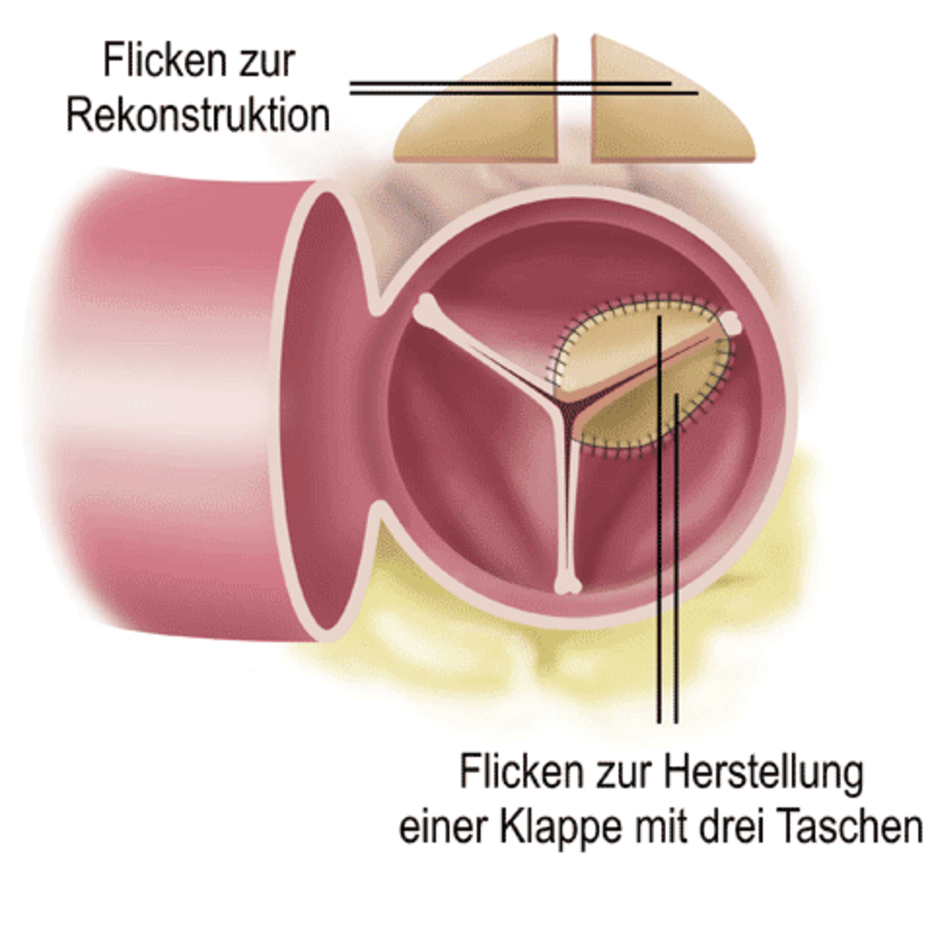
Bicuspid aortic valve
Approximately one per cent of all people are born with a so-called bicuspid aortic valve. This anatomical anomaly occurs more frequently in certain families. Men are affected twice as often as women. Normally, the aortic valve consists of three valve parts. In people with a bicuspid aortic valve, two of the three valve cusps have fused together, so that their aortic valve consists of two parts of different sizes.
This structural change leads to premature calcification, thickening and narrowing of the aortic valve. The ascending aorta following the aortic valve is often thin-walled. All these factors increase the risk of aortic aneurysm and dissection.
Illustration of aortic valve stenosis (narrowing) before surgery.
© www.IDHK.de 2012 (Illustration Jan Bazing)
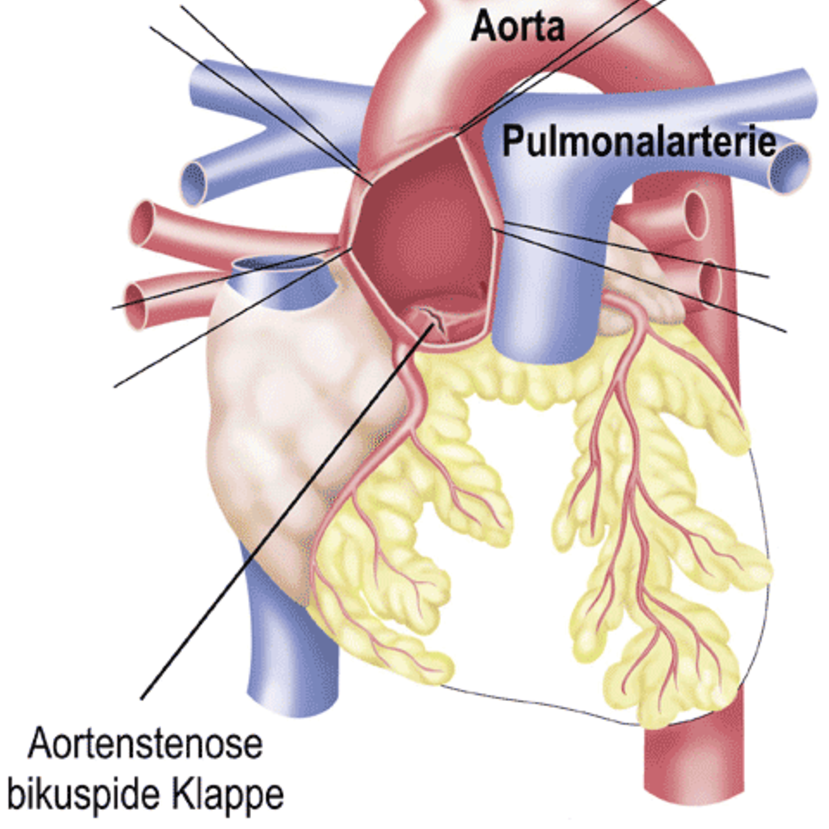
Aortic stenoses
Congenital narrowing (stenosis) of the aorta can cause a wide range of symptoms. The narrowing can be more or less pronounced. In the case of coarctation of the aorta, there is a congenital narrowing in the area of the aortic arch or at the end of the aortic arch. This anatomical abnormality occurs in seven per cent of all congenital heart defects and in up to 20 per cent of all patients with Turner syndrome.
The mid-aortic syndrome is a very rare condition that has been described in genetic diseases (Alagille syndrome, Williams-Beuren syndrome).
In 60 per cent of cases, it occurs without any identifiable cause (idiopathic). Mid-aortic syndrome is also referred to as abdominal aortic coarctation because the abdominal aorta and its large vessel outlets are narrowed. Before and after the constriction, the aortic wall can widen and weaken (aortic aneurysm). In conjunction with high blood pressure, there is an increased risk of aortic dissection.
Genetic diseases
In the case of genetic connective tissue disorders, collagen and elastin with an altered structure are formed, which weakens the three-layer wall structure of the aorta. This results in widening and thinning of the aortic wall (aneurysm), tears (dissections) or complete ruptures (ruptures) of the vessel wall.
Marfan syndrome affects both men and women. Every year, one in 3,000 children is born with this hereditary connective tissue disease. The gene mutation affects the FBN1 gene, which causes the production of a structurally weak version of the protein fibrillin-1. The connective tissue that is formed by this protein is considerably weaker than in people without this genetic peculiarity. This weakness in the connective tissue primarily affects joints, tendons, the eye and the aortic wall.
Over time, 95 per cent of those affected develop heart valve disease (aortic valve insufficiency), thoracic aortic aneurysm or aortic dissection. It is not only the changes in the aorta itself that increase the risk of aortic complications. Anatomical changes to the rib cage (funnel chest, pigeon chest) and to the spine (kyphoscoliosis) can also contribute to an aortic dissection due to altered pressure and tensile forces.
Turner syndrome is a genetic disorder caused by the loss or failure of one of the X chromosomes. Only women are affected. Every year, one in 3,000 newborn girls has this condition in their genetic makeup. The severity of the symptoms can vary depending on the genetic findings, and is associated with short stature, renal malformations, and absent puberty.
The risk of aortic disease (aortic aneurysm, dissection, rupture) is increased due to genetic vascular abnormalities. Patients with Turner syndrome are more likely to have a bicuspid aortic valve.
The Ehlers-Danlos syndrome describes a group of inherited connective tissue disorders that can affect both men and women. Approximately one in 50,000 children is born with this genetic condition each year. There are several genetic defects that affect collagen metabolism.
Collagen is a structure-providing protein. The defective version of the protein leads to the hypermobility and hyperextensibility of the joints that are typical of the syndrome. Both the skin and blood vessels of those affected are very vulnerable. Four per cent of these patients experience aortic dissection or rupture, which can occur spontaneously without the prior formation of an aortic aneurysm.
One in 100,000 children is born with this genetic condition every year. Loeys-Dietz syndrome is caused by mutations in two genes. The syndrome is clinically similar to Marfan syndrome, but the eyes are not affected. As with Ehlers-Danlos syndrome, the skin is easily damaged. A characteristic feature is the presence of a cleft palate or a split uvula (uvula bifida).
The malformations in the blood vessel system are extensive in those affected. Arteries that are dilated or stretched in places run throughout the body, in which aneurysms form over time. Typical are tortuous arteries, which occur particularly in the neck area. In 95 per cent of those affected, an aneurysm is found in the area of the aortic root.
Diagnosis
There are various ways to examine and visualise the aorta. Depending on the aortic disease and treatment option, further examinations may be necessary. Some of these important examinations are explained below.
You can find a list of the most important methods on our Diagnostics page.
Treatment of aortic diseases
In many cases, immediate surgical treatment is required when an acute aortic disease is diagnosed. However, it is not uncommon for aortic diseases to develop slowly and even without symptoms over a longer period of time. Once they have been detected, they only require close monitoring and the avoidance of risk factors. While the ascending part of the aorta is only operated on ‘conventionally’ (open surgery), ‘interventional’ care (TEVAR; thoracic endovascular aortic repair) of the descending aorta is now standard.
You can find out more about the various treatment options on the pages about aortic aneurysm and the page about aortic dissection.
Aortic surgery
Detailed and easy-to-understand information on surgical techniques and methods can be found on the page about aortic surgery.
Outpatient clinic and consultation
Aortic consultation at the cardiosurgical outpatient clinic at the Deutsches Herzzentrum der Charité (DHZC):
Tel +49 30 4593-2002
Marfan Centre of the Charité and the DHZC:
Outpatient clinic for patients with genetic aortic diseases
Tel +49 30 450 665 356
E-mail: marfan@charite.de
Offers for medical professionals
The Deutsches Herzzentrum der Charité is the most experienced centre in the Berlin / Brandenburg region for the treatment of acute aortic dissections, performing the highest number of procedures per year in the region of Berlin / Brandenburg. With a catchment area of over six million inhabitants, this is a great responsibility. The pre-clinical management of aortic emergencies is an important component in the care of affected patients. There is a great deal to be organised in advance before the patient arrives at the Deutsches Herzzentrum der Charité.
A central hotline for aortic emergencies has been set up specifically for this purpose in the region. The team of the aortic telephone is staffed around the clock by experienced specialists, provides important information to the referring colleagues in the care of aortic emergencies and organises the further course of action up to surgical care.
The aortic telephone can be reached at (030) 4593 2007.
The concept has led to a significant improvement in diagnostics and care: the number of patients operated on at DHZC for acute type A aortic dissection has increased by more than 45 percent compared to previous years. The time from diagnosis to surgery has also been significantly reduced. Overall, mortality has also decreased.
Together with the health app DoctorBox, the DHZC has introduced an emergency ID card for aortic patients. This provides emergency doctors and paramedics with quick access to the patient file in an emergency.
Patients who wish to take advantage of this service can register using the free DoctorBox app and enter data on their blood type, illnesses and allergies. Clinics or doctors' offices can also use this app to transmit patient data.
Once the medical data has been stored, the emergency ID card can also be activated. In an emergency, emergency doctors or members of a hospital emergency room team can access the DoctorBox website via a QR code printed on the card and, after entering a PIN, can access all of the patient's health data.
In addition, the number of the DHZC aortic hotline is printed on the card, enabling emergency rooms and emergency doctors to get quick support.


